Drug-induced Acute Hepatic Failure
Sanjay Kakar, MD
Key Facts
Terminology
Onset of hepatic encephalopathy within 8 weeks of onset of symptoms
INR is > 1.5, and there is no evidence of chronic liver disease
Corresponding pathologic terms: Massive/submassive necrosis, fulminant hepatitis
Clinical Issues
Acetaminophen is most common cause of ALF in USA, accounting for 40-50% of cases
Microscopic Pathology
Massive/submassive necrosis with little or no inflammation: Acetaminophen, most toxins
Massive/submassive necrosis with prominent inflammation: Most idiosyncratic drug reactions
Microvesicular steatosis: Tetracycline, zidovudine
Regenerative nodules can be seen later in course of disease and can be mistaken for cirrhosis
Unlike fibrous septa of cirrhosis, necrotic areas show pale staining with trichrome stain and lack elastic fibers on elastic stain
Top Differential Diagnoses
Necrosis with inflammation: Acute viral hepatitis A and B, autoimmune hepatitis, Wilson disease
Necrosis with minimal inflammation: Herpes simplex and adenoviral hepatitis, acute ischemia, acute Budd-Chiari syndrome
Microvesicular steatosis: Alcoholic foamy degeneration, acute fatty liver of pregnancy, Reye syndrome, Jamaican vomiting sickness, rare metabolic disorders like carnitine deficiency
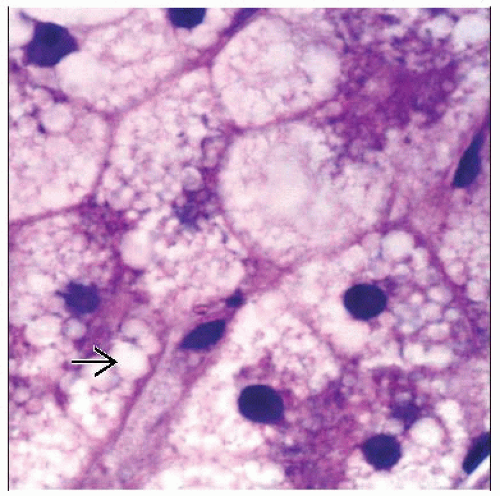
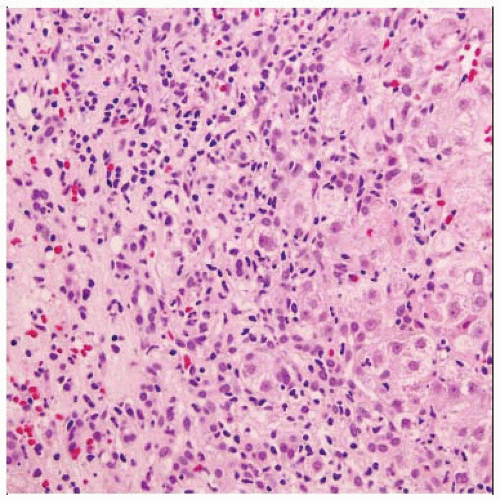 H&E of acute liver failure shows confluent necrosis with lymphoplasmacytic inflammation (left). Swelling and inflammation are seen in the remaining parenchyma (right). |
TERMINOLOGY
Abbreviations
Acute liver failure (ALF)
Definitions
Hepatic encephalopathy and reduced synthetic function evidenced by INR > 1.5
Duration of disease less than 26 weeks
Absence of chronic liver disease
Corresponding pathologic term is massive/submassive necrosis or fulminant hepatitis
ETIOLOGY/PATHOGENESIS
Mechanisms of Injury
Massive/submassive necrosis due to intrinsic hepatotoxins
Most toxins fall in this category
Carbon tetrachloride, mushroom poisoning, recreational drugs like cocaine and MDMA (ecstasy)
Very few drugs cause this pattern of injury
Acetaminophen, halothane
Herbal medications: Pennyroyal, glue thistle, germander
Massive/submassive necrosis due to idiosyncratic injury
Most drugs fall in this category
Drugs used for treatment of tuberculosis such as isoniazid are one of leading culprits of ALF in developing world
Other implicated drugs: Monoamine oxidase inhibitors, anticonvulsants (valproate, phenytoin), antimicrobial agents (sulfonamides, cotrimoxazole, ketoconazole)
Diffuse microvesicular steatosis due to acute mitochondrial injury
Presents as ALF without histological necrosis
Commonly implicated drugs: Tetracycline, zidovudine, valproic acid, amineptine
CLINICAL ISSUES
Presentation
Depends on specific drug or toxin
Acetaminophen is most common cause of ALF in USA accounting for 40-50% of cases
Dose-dependent toxicity occurs with accidental (1/3 of cases) or suicidal (2/3 of cases) overdose
Minimum toxic dose in adults is 7.5-10 g, but severe liver damage occurs with ingestion of 15-25 g
Chronic alcohol consumption, obesity, and drugs that induce P-450 cytochrome system can lower toxic threshold of acetaminophen
Gastrointestinal symptoms for first 12-24 hours and latent phase of 24-48 hours is followed by ALF 72-96 hours after drug ingestion
Treatment
Drug withdrawal, supportive care, and liver resuscitation (hypothermia, albumin dialysis, artificial liver support)
Liver transplantation is often necessary
Acetaminophen hepatotoxicity can be prevented with acetyl-cysteine therapy within 12 hours of drug ingestion
Prognosis
Severe encephalopathy and older age are adverse prognostic factors for spontaneous recovery
For acetaminophen toxicity, blood levels 4-16 hours after ingestion are best predictor of outcome; highest mortality is encountered in late presenters
MICROSCOPIC PATHOLOGY
Histologic Features
Based on pattern of injury, drug-induced ALF can be divided into 4 categories
Massive/submassive necrosis with little or no inflammation
Extensive confluent hepatocellular necrosis
Necrosis may be nonzonal, centrizonal (acetaminophen, halothane, carbon tetrachloride), midzonal (beryllium), or periportal (cocaine, ferrous sulphate)
Concomitant steatosis, often microvesicular, can be present (carbon tetrachoride poisoning, cocaine)
Mild or absent inflammation
Massive/submassive necrosis with prominent inflammation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree