Direct-to-Implant Breast Reconstruction
Amy S. Colwell
DEFINITION
Mastectomy is increasingly performed for breast cancer treatment or risk reduction in high-risk patients. The goal of breast reconstruction is to rebuild the breast and restore a sense of normalcy.
ANATOMY
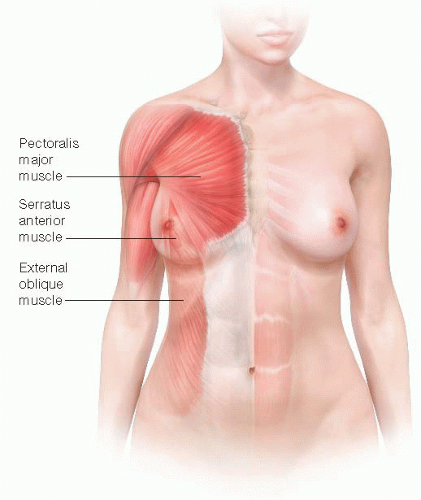
The breast glandular tissue extends to the clavicle superiorly, the inframammary fold (IMF) inferiorly, sternum medially, and latissimus dorsi laterally (FIG 1). With a skin-sparing or nipple-sparing mastectomy, the glandular tissue is removed and the skin is spared, thus making direct-to-implant breast reconstruction possible. In implant-based breast reconstruction, a space is created underneath the pectoralis muscle, and the serratus anterior is sometimes used to help define the lateral border of the reconstructed breast (FIG 2).
NATURAL HISTORY
PATIENT HISTORY AND PHYSICAL FINDINGS
Patient selection in immediate direct-to-implant breast reconstruction is one of the keys to success. A history is obtained to check for comorbidities that are known risk factors for increased complications including smoking, diabetes, body mass index (BMI), and previous breast radiation. On physical exam, the breast is assessed for skin quality, size, scars from previous procedures, symmetry, position of the IMF, and nipple position if a nipple-sparing mastectomy is being considered.
DIFFERENTIAL SURGICAL TREATMENT OPTIONS
Two-stage tissue expander-implant reconstruction
Autologous reconstruction using tissue from the body including the abdomen (TRAM, transverse rectus abdominis myocutaneous; DIEP, deep inferior epigastric perforator; SIEA [superficial inferior epigastric artery] flaps), buttocks (SGAP, superior gluteal artery perforator; IGAP [inferior gluteal artery perforator] flaps), thighs (TUG [transverse upper gracilis] flap), and back (latissimus dorsi)
Fat transfer
No, or delayed, reconstruction
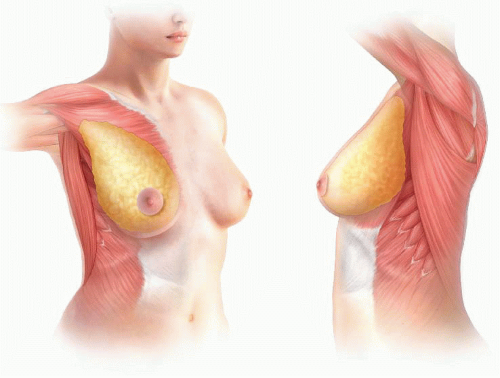 FIG 1 • The anatomic boundaries of the breast are the clavicle, sternum, inframammary fold, and latissimus dorsi. |
NONOPERATIVE MANAGEMENT
Breast reconstruction is a choice, and patients undergoing mastectomy may not elect to pursue reconstruction. If no reconstruction is planned, the breast skin is closed and the chest remains flat in contour. If desired, external breast prostheses are available for women to wear in their clothing to give the appearance of a breast.
SURGICAL MANAGEMENT
The goals of reconstruction are considered in determining if the reconstruction is designed to augment, reduce, or maintain the current breast size. In general, if a woman wants a significant increase in breast size, this is more safely done in two stages using a tissue expander followed by exchange to implant in a second surgery (see Part 5, Chapter 15). For single-stage implant reconstruction, the implant is placed directly in a partial subpectoral pocket in order to allow superior soft tissue coverage with muscle in the cleavage area of the breast and to help prevent contracture around the implant.4 The implant is subcutaneous inferiorly, which allows a more natural teardrop shape, and is typically supported by a surgical acellular dermal matrix (ADM) or mesh. Currently, the most common ADM is AlloDerm (human dermis, LifeCell, Branchburg, NJ), but a variety of ADM or mesh material derived from human dermis, porcine dermis, bovine pericardium, fetal bovine dermis, silk, titanium, and Vicryl exist.
Preoperative Planning
With immediate implant reconstruction, a foreign body (implant) is placed into a skin envelope that has been partially devascularized with the mastectomy. Therefore, sterility is an important component of preoperative planning and operative management. The patient sits upright and is marked prior to the procedure. Important landmarks include the IMF position, its relation to the IMF on the contralateral breast, and the lateral border of the breast. The mastectomy portion of the procedure is performed first followed by the reconstruction.
Positioning
The patient is positioned supine with the arms secured on arm boards at the side, angled approximately 80 to 85 degrees from the operating table (FIG 3). This allows access to the axillary lymph nodes for sampling during the mastectomy. Both breasts are prepped and draped into the field.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree