Digit Amputations
Steven C. Haase
DEFINITION
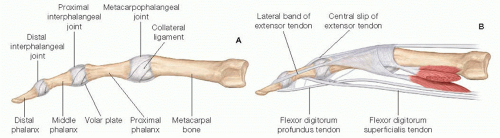
Digital amputation refers to the removal of a finger or thumb, most commonly at the level of the phalanges or interphalangeal joints (FIG 1). More proximal amputations that include a significant portion of the metacarpal are referred to as ray amputations. The techniques found in this chapter have been described chiefly for the hand, although similar procedures can be used on the foot in many cases.
Digital or ray amputation may be indicated for subungual melanoma, or for other large, invasive melanomas of the finger or thumb.
PATIENT HISTORY AND PHYSICAL FINDINGS
It is important to assess how long the lesion has been present; how fast it has grown; and whether there has been any history of ulceration, bleeding, or pain. Lesions exhibiting rapid growth in addition to these other findings may require more aggressive treatment.
A patient’s age, handedness, occupation, and hobbies should be considered carefully in planning an operation that might significantly affect their function. In some cases, preoperative consultation with a physiatrist and/or occupational therapist may help a patient mentally prepare for what is a sometimes emotionally difficult operation.
Physical examination should include both the epitrochlear and axillary lymph nodes. For lesions on the toes, examination should include the popliteal and inguinal basins. Clinically node-negative patients with melanoma greater than or equal to 1 mm in thickness, or thin lesions with other worrisome histologic features, may be candidates for sentinel lymph node biopsy at the time of amputation. (see Part 5, Chapter 27). Patients with clinically involved nodes should undergo fine needle aspiration (FNA) biopsy and staging for distant metastases. These patients may require lymph node dissection at the time of amputation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Suspicious lesions require biopsy to establish diagnosis. This should include a full-thickness sampling of the skin and/or nail matrix for accurate assessment of depth of the lesion. Increased depth of invasion is consistently associated with worse prognosis.1
For large or fixed lesions, radiographs of the digit should be obtained to assess for the presence of bone involvement. If radiographs demonstrate significant bone destruction, additional imaging with magnetic resonance imaging (MRI) may be required to assess the full extent of tumor spread in the hand.
SURGICAL MANAGEMENT
Positioning
For hand operations, patients are positioned supine, with the affected extremity extended on a hand table attached to the operating room table.
TECHNIQUES
DIGITAL AMPUTATION
Skin Incision
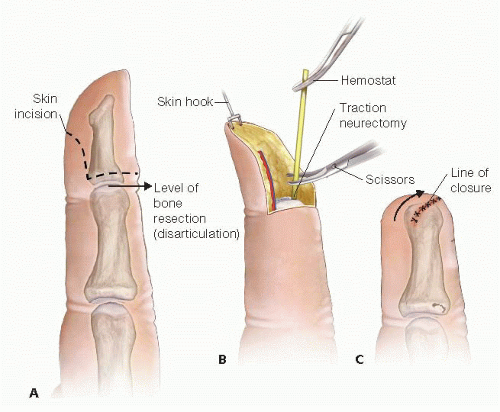
The skin incision should be designed as a “fish mouth,” such that dorsal and volar flaps are created that close in a more or less transverse line of closure that gives a smooth, rounded contour to the amputation stump.
The skin flaps should be designed with enough laxity to close over the underlying skeleton to be preserved. Typically, the level of disarticulation or osteotomy should be a few millimeters proximal to the level of the skin incision.
Ideally, the volar flap can be designed a bit longer than the dorsal flap (FIG 2A) to allow resurfacing of the entire
opposition surface (contact surface) of the fingertip with the thicker, more densely innervated palmar skin.
Soft Tissue Dissection
The soft tissue should be divided in a way that minimizes devascularization of the tissues or skin flaps. Sharp scalpel dissection directly to the bone can be performed both dorsally and volarly, dividing the neurovascular bundles, tendons, and periosteum.
Bone Dissection and Osteotomy
The periosteum should then be sharply elevated proximally using an elevator or scalpel, circumferentially around the digit. This will allow the bone cut to be positioned slightly proximal to the soft tissue dissection.
Bone division is most efficiently accomplished with a small oscillating power saw. Instruments such as bone cutters or rongeurs tend to crush and fracture the proximal bone stock and are not recommended.
If disarticulation is planned, the collateral ligaments should be detached from the proximal aspect of the joint, so this bulky, poorly vascularized tissue is discarded with the amputated part.
Traction Neurectomy
The neurovascular bundle should be identified with delicate dissection. The artery may be cauterized; the nerve should be dissected away from the artery and followed proximally several millimeters. The nerve should be placed on traction, divided proximally, and allowed to retract (FIG 2B). This will ensure that the neuromas that inevitably form at the end of each digital nerve will be located proximally to the contact surface of the fingertip.
Closure
Closure is usually performed with a single layer of nonabsorbable sutures (FIG 2C), which are removed about 2 weeks later. Do not suture the extensor tendon to the flexor tendon over the end of the exposed bone; this will functionally shorten the flexor tendon to that digit, resulting in weakened grip strength due to the quadrigia effect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree