De Novo Membranous Glomerulonephritis
Anthony Chang, MD
Key Facts
Clinical Issues
0.5-9% of kidney transplant patients
Proteinuria
Renal dysfunction
Unfavorable prognosis
2/3 of patients eventually require renal replacement therapy
Microscopic Pathology
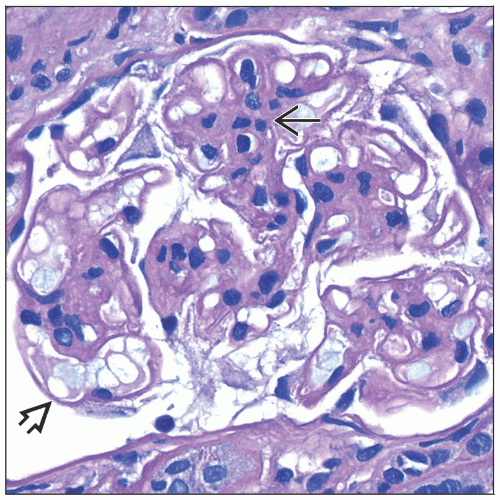
Glomerular basement membrane thickening, diffuse or segmental
GBM “spike” formation
Granular IgG staining in glomerular capillary walls
C4d and C3 may also stain glomerular capillaries in similar pattern
Careful evaluation of C4d glomerular staining pattern is critical if this is only antibody tested in transplant kidney biopsies
C4d in peritubular capillaries found in ˜ 70% of cases
Subepithelial electron-dense deposits seen by electron microscopy ± basement membrane “spike” formation
Mesangial hypercellularity in 1/3 of cases
Spikes of GBM on silver or PAS stains, ± “Swiss cheese” appearance depending on stage of MGN
Ancillary Tests
IgG1 is predominant or codominant subclass
Top Differential Diagnoses
Recurrent MGN
Chronic transplant glomerulopathy
TERMINOLOGY
Abbreviations
Membranous glomerulonephritis (MGN)
Synonyms
Membranous glomerulopathy, de novo
Membranous nephropathy, de novo
Membranous glomerulonephropathy, de novo
Definitions
MGN in kidney allograft when primary cause of end-stage renal disease is not MGN
ETIOLOGY/PATHOGENESIS
Allo-/Autoantibody
May represent unusual manifestation of chronic antibody-mediated rejection
Can occur in HLA identical grafts, presumably due to non-HLA antigen
Rat model of de novo MGN occurs only in transplant and not native kidney
One autopsy showed de novo MGN involving only kidney allograft without MGN in native kidneys
One de novo MGN case with donor-specific antibodies against HLA-DQ7
Association with C4d deposition in peritubular capillaries and anti-HLA-DQ
No autoantibodies to phospholipase A2 receptor (PLA2R)
CLINICAL ISSUES
Epidemiology
Incidence
0.5-9% of kidney transplant patients
Presentation
Typically manifests late (> 3 years)
Renal dysfunction
Proteinuria
2nd most common cause of proteinuria in renal allograft patients
Often nephrotic range (> 3 g/24 hours), may be intermittent or persistent
Treatment
Not well defined
Prognosis
Unfavorable
5-year graft loss of 50% or more
2/3 eventually progress to renal failure
De novo MGN may recur in subsequent renal allografts
MACROSCOPIC FEATURES
General Features
Renal vein thrombosis occasionally present
Less common than with idiopathic MGN in native kidneys
MICROSCOPIC PATHOLOGY
Histologic Features
GBM thickening
Focal &/or segmental thickening common
Glomerular capillaritis in ˜ 50%
Increased leukocytes within glomerular capillaries
Mesangial hypercellularity in ˜ 33%
Double contours or duplication of GBM in 50%
Possibly due to concurrent chronic transplant glomerulopathy (chronic antibody-mediated rejection)
Prominent interstitial inflammation
Often sufficient for diagnosis of acute (T-cell-mediated) rejection
Intimal arteritis
Acute (type 2) rejection found in subset
ANCILLARY TESTS
Immunofluorescence
Positive granular capillary wall staining for IgG, kappa and lambda light chains
IgG1 is predominant or codominant subclass
IgG4 is predominant subclass in primary (or recurrent) MGN
Variable capillary wall staining for C4d, C3, C1q, and IgM
C4d(+) peritubular capillary deposition in ˜ 70%
Electron Microscopy
Transmission
Subepithelial amorphous electron-dense deposits
Often small and relatively sparse
Stage I (Ehrenreich-Churg) deposits common
Duplication of GBMs
Subendothelial space widening when injured endothelial cells detach from GBM
DIFFERENTIAL DIAGNOSIS
Recurrent MGN
Clinical history of MGN as original disease
Earlier onset (< 3 months)
Autoantibodies to PLA2R
IgG4 predominant
Donor-Derived MGN
Present in donor biopsy, disappears in a few months
Chronic Transplant Glomerulopathy
Duplication of GBM without immune complexes
Occurs concurrently in 50% of de novo MGN cases
C4d(+) in peritubular capillaries
Multilamination of peritubular capillary basement membranes on EM
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree