These tests are only as good as the specimen received.
Specimens collected from patients in isolation should be clearly labeled on the specimen container and requisition form with appropriate warning stickers. The specimen container should then be placed inside two sealed, protective biohazard bags before it is transported to the laboratory.
The U.S. Occupational Safety and Health Administration (OSHA) requires that all specimens be placed in a secondary container before transportation to the laboratory. Most laboratories prefer plastic biohazard bags. Requisitions should be kept on the outside of the bag or in a separate compartment in the biohazard bag, if available.
Inflammatory
Benign
Atypical
Suspicious for malignancy
Positive for malignancy (in situ versus invasive)
TABLE 11.1 Nucleic Acid Testing Performed in Gynecologic Cytology | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Grade I: tumors showing a marked tendency to differentiate; 75% or more of cells differentiated
Grade II: 75% to 50% of cells differentiated, slight to moderate dysplasia and metaplasia
Grade III: 50% to 25% of cells differentiated, marked dysplasia, marked atypical features, and cancer in situ
Grade IV: 25% to 0% of cells differentiated
Use local anesthesia in most cases. Aspirate superficial or palpable lesions without radiologic aid, but aspirate nonpalpable lesions using radiographic imaging as an aid for needle placement. Use sterile technique.
Position the needle properly, then retract the plunger of the syringe to create negative pressure. Move the needle up and down, and sometimes at several different angles. Release the plunger of the syringe and remove the needle.
Express material obtained onto glass slides, which must either be fixed immediately in 95% alcohol, spray-fixed, or air-dried, depending on the staining procedure used by the laboratory. The remaining material may be placed in a preservative solution, such as 50% alcohol. Check with your laboratory for recommended fixation requirements. Material may also be sent to the laboratory in the syringe.
Record the source of the sample and method of collection so that evaluation can be based on complete information.
Clearly label specimens collected from patients in isolation on the specimen container and on the requisition form with an appropriate warning sticker. Place the specimen container inside two sealed, protective biohazard bags before transport.
See Chapter 1 guidelines for intratest care.
Infectious processes. The infectious agent may be seen, or characteristic cellular changes may indicate the infectious agent that is present.
Benign conditions. Some characteristic cellular changes may be present, indicating the presence of a benign process.
Malignant conditions, either primary or metastatic. If the disease is metastatic, the findings may be reported as consistent with the primary malignancy.
Explain the purpose, procedure, benefits, and risks of the test. Even though a local anesthetic is used, the procedure causes some discomfort, and this should not be minimized. If the approach involves passing near a rib, the pain may be greater because of the sensitivity of the bone; this is not a cause for alarm. Unexpected pain may induce a vasovagal or other undesirable response. Other risks include infection and hematoma or hemorrhage, depending on the site aspirated.
See guidelines in Chapter 1 for safe, effective, informed pretest care.
Monitor for signs of inflammation and use site care infection control measures. Treat pain, which may be common in sensitive areas such as the breast, nipple, prostate, and scrotum. Monitor for specific problems, which vary depending on the site aspirated (e.g., hemoptysis after a lung aspiration).
Counsel about follow-up procedures for infections and malignant conditions.
Follow guidelines in Chapter 1 for safe, effective, informed posttest care.
node is free of disease, the rest of the nodes in the patient will also be free of disease. Three methods (along with marking of the skin) are used: (1) lymphoscintigraphy (preoperative), (2) nuclear probe localization (intraoperative), and (3) blue dye injection (intraoperative). Often, all three techniques are used together, the lymph nuclear scan being the most common (see Procedures).
Lymph nuclear scan (lymphoscintigraphy)
For the breast, inject the radiopharmaceutical (large volume) subcutaneously into the breast and adjacent to suspected breast tumor; for lymphedema, inject into webs of fingers and toes.
For melanoma, make four to six intradermal injections around the tumor or excision site, avoiding scar tissue.
Perform immediate imaging with the patient in the position expected during surgery.
Nuclear radiation (gamma) probe (which produces sound)
Remember that a previously administered radiopharmaceutical and the sound radiation detector permit node detection and localization to determine where the initial operative incisions can be made.
Use the sound-radiation gamma probe to locate the area of radioactivity not associated with the injection sites. Of the three procedures, the probe is the most sensitive.
Blue dye (not externally visible)
In order to identify the nodes to undergo biopsy, inject the feet in the web between the toes and the hands between the second and third fingers (allergic reaction to the dye may occur).
Remember that an operative biopsy procedure follows.
 PROCEDURAL ALERT
PROCEDURAL ALERT
Abnormal findings reveal metastatic nodes and routes of spread.
Asymmetry may indicate lymph flow obstruction.
Explain purpose of sentinel node identification procedures.
Inform the patient that if the results are positive, surgery usually follows soon after.
Be aware that usually, sedation or analgesia is not ordered.
Mark the site of lymph nodes with indelible pen.
Provide support, assist with positioning, and assure the patient that testing is proceeding as expected.
Monitor injection site (breast, toes, fingers, or around tumor excision site). Check for signs of inflammation or bleeding.
If surgery is planned, prepare according to established protocol. Also, see Biopsies Overview in alphabetical listing.
When surgery is scheduled, take images just before transfer to the operating room (2 hours later or next morning).
Counsel about outcomes and possible need for further testing or treatment.
Extreme drug resistance (EDR) assay tests of solid tumors and malignant fluids (blood, bone marrow effusions), which determine the probability of a tumor’s resistance to specific chemotherapeutic drugs (e.g., 5-fluorouracil [5-FU] for colon cancer). If the tumor cells grow in the presence of extreme exposures to a specific drug, this indicates the presence of significant drug resistance and, by identifying inactive agents, avoids exposing patients to the toxicity of drugs that are likely to be ineffective, saves valuable treatment time, and decreases the possibility of cross-resistance to other effective agents.
Differential staining and cytotoxicity (DiSC) assay uses special stains and techniques to detect drug resistance in leukemia, lymphoma, blood, and bone marrow specimens.
Prognostic markers measure the tumor’s growth potential or ability to invade other tissues (metastasis). Tumor cells release proteases and angiogenic factors to break down basement membranes and induce new vascularization of the tumor, which delivers oxygen and nutrients to the tumor and allows micrometastasis to distant sites.
Predictive markers identify specific mechanisms of drug resistance and provide information on how effective clinically indicated chemotherapy agents will be in treating the patient’s tumor cells. Prognostic and predictive markers use molecular probes to determine the genetic characteristics, amount of protein, proliferation index, resistance mechanisms, receptor status, and other defining factors of the patient’s malignant tumor. To obtain the most comprehensive analysis of the patient’s unique tumor biology, drug resistance testing is done in combination with oncoprofiles and prognostic and predictive markers for the specific cancer type. A radiation resistance assay can also be done before the treatment actually begins.
Androgen receptor. This receptor predicts prostate cancer’s response to hormone therapy.
Angiogenesis index (p53, Tsp-1, CD31). The AI defines a patient’s risk for occult metastatic disease and is composed of factors that characterize the capacity for new blood vessel formation: p53, Tsp-1, and CD31 (vessel count). The p53 gene contributes to tumor growth suppression by slowing cell cycle progression and promoting apoptosis in damaged tumor cells. It also suppresses tumor angiogenesis. Tsp-1 levels have been found to decrease after the tumor sustains mutations in p53. CD31 is expressed on the membrane of endothelial cells, allowing for microvessel count in the tumor.
BAX. Increased levels of BAX, a 21-kd protein and amino acid, indicate accelerated programmed cell death induced by apoptotic stimulus.
Proto-oncoprotein bcl2 (apoptosis regulator). The translocation of the bcl2 gene, occurring in follicular lymphomas, is brought under control of the immunoglobulin gene promoter, resulting in increased intracellular levels of bcl2 protein. This protein suppresses programmed cell death (apoptosis). Induction of cell death is an important mechanism for many chemotherapeutic agents. An abnormal expression of bcl2 protein can render tumor cells resistant to chemotherapeutic agents.
Cathepsin D (invasion potential). Cathepsin D, a lysosomal acid protease, has been associated with metastatic potential. Elevated levels of cathepsin D are predictors of early recurrence and death in node-negative cancer and breast cancer.
CD31 (component of tumor angiogenesis index). CD31 stains microvessels, allowing for counting, and helps to predict more aggressive disease, metastases, poor survival, and new vascularization of the tumor mass.
DNA ploidy and S phase (flow cytometry). DNA ploidy and proliferative index are independent indicators of prognosis. Patients with aneuploid tumors or high S-phase fractions have poor disease-free survival compared with patients with diploid or low S-phase fraction tumors. DNA ploidy (image analysis) (Feulgen stain) is an indicator of prognosis in selected tumor types in fresh specimens.
Epidermal growth factor receptor (EGF-R). This growth factor receptor is a glycoprotein tyrosine kinase, either EGF or transforming growth factor-α (TGF-α). When high levels occur in breast, prostate, ovarian, lung, and squamous cell carcinomas, there is an association with poorer prognosis and poor disease-free survival.
Endoglin (CD105). Endoglin normally occurs in vascular endothelial cells of capillaries, arterioles, small arteries, and venules. Increased levels are found in tumor vessels and proliferating endothelial cells. Endoglin has been found in non-T/non-B and pre-B acute lymphoblastic leukemia (ALL) and acute myelocytic and myelomonocytic leukemia cells.
Estrogen receptor (ER) and progesterone receptor (PR). ER and PR positivity is associated with a 70% response rate to antihormonal therapy. In contrast, the response rate is less than 10% among
patients whose tumors are ER and PR negative. Patients whose tumors are ER and PR positive generally achieve superior disease-free survival.
Glutathione S-transferase (GST); alkylator resistance. GST is an enzyme that inactivates certain anticancer agents by linking glutathione to the drug. Increased GST levels are associated with tumor resistance to chlorambucil and melphalan.
HER2/neu c-erbB2 oncoproteins. The presence of HER2/neu, a protein that functions as an oncogene, is associated with poorer prognosis. HER2/neu detection also provides information on the potential treatment response to trastuzumab (Herceptin).
Ki-67 (proliferative index). This is a staining technique. Monoclonal antibody Ki-67 is associated with increased cell proliferative activity in tumors and with more aggressive tumors and poor disease-free survival.
MDR-1 (P170 glycoprotein: multidrug resistance). The presence of MDR-1 cancer cells is associated with resistance to naturally produced chemotherapeutic agents such as paclitaxel (Taxol), doxorubicin, and etoposide and plays a critical role in the selection of a treatment regimen.
O6-methylguanine-DNA methyltransferase (MGMT) (nitrosourea resistance). MGMT, a repair protein, occurs after DNA damage caused by nitrosoureas, such as BCNU. Brain cancer patients with high levels of the MGMT gene and alkyltransferase (AT) have shorter disease-free and overall survival.
Multidrug resistance protein (MRP). This protein is similar to, but distinct from, MDR-1 and is strongly associated with resistance to cisplatin drugs in ovarian cancer.
p21. A protein-like tumor suppressor like p53, p21 controls when and how the cell replicates. Low levels of p21 are associated with increased risk for tumor occurrence, and the absence of p21 contributes to aggressive growth in some tumors.
p53 (cell cycle and Tsp-1 regulator). The tumor suppressor gene p53 regulates cell cycle progression, cellular proliferation, DNA repair, apoptosis (cell death), and angiogenesis. Increased levels of mutated p53 protein in tumor cell nuclei are associated with tumor progression and a poorer prognosis.
PCNA (proliferative index). Presence of PCNA protein is associated with cell proliferation, and increased levels occur with more aggressive tumors and are associated with poor disease-free survival.
Thymidylate synthase (TS; 5-FU resistance). Drug resistance tests of thymidylate synthase (TS), a cellular enzyme essential for DNA biosynthesis and cell proliferation that is a target for 5-FU, is an important component of some breast cancer and colon cancer treatment regimens. Increased TS expression correlates with poorer response rates to 5-FU and with shorter survival in breast and colon cancer.
Thrombospondin-1 (Tsp-1). This extracellular matrix protein is involved in wound healing. Low value is associated with increased tumor neovascularity and mutant p53 expression.
UIC-2 (MDR-1) shift assay. This staining technique can be performed on solid tumors. The UIC-2 shift assay can be performed on blood and bone marrow specimens from patients with acute myelogenous leukemia (AML), multiple myeloma, or lymphoma and, if the sample contains an adequate amount of viable tumor cells, on solid tumors.
Vascular endothelial growth factor (VEGF). Vascular endothelial growth factor, or vascular permeability factor (VPF), plays an important role in angiogenesis, which promotes tumor progression and metastasis.
TABLE 11.2 Useful Information From a Single Biopsy Specimen* | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
Explain the purpose and biopsy procedure and obtain a signed, witnessed consent form.
Remember that patient preparation depends on the predetermined biopsy site. Complete blood count (CBC), prothrombin time (PT), and other bleeding time determinants may be required. Obtain a pertinent history (e.g., prior radiation therapy, other cancer, current medications, pregnancy).
Follow Chapter 1 guidelines for safe, effective, and informed pretest care.
Monitor for signs of bleeding, inflammation, infection, laceration of tissue and organs, and perforation. Treat pain, which may be experienced to various degrees depending on the body site sampled.
Counsel the patient about follow-up procedures and treatment for infections and malignant conditions.
Follow the guidelines in Chapter 1 for safe, effective, and informed posttest care.
ER and PR. These hormone receptors are indicators of prognosis and are used to manage hormonal therapy in breast and endometrial cancer. Immunohistochemical (IHC) staining aids recognition of metastatic breast cancer.
DNA ploidy. This test measures cell turnover or replication; it is used to predict prognosis and shorter survival times by the presence of aneuploid (rapidly replicating cells) for certain tumor types, such as breast, prostate, and colon; it is less clear for ovarian, lung, kidney, and bladder (urine) tumors (66% of breast cancers are aneuploid).
S-phase fraction (SPF)—to predict survival and reduced chance of relapse. Low levels of SPF appear to have longer survival and reduced chance of relapse. SPF is the DNA synthesis phase obtained by a statistical method.
Cathepsin D—done to determine prognosis. The presence of this lysosomal protease is estrogen related and may promote tumor spread. Prognostic significance remains ambiguous.
EGF reception—done to predict survival time. Presence is correlated with ER negativity, aneuploidy, increased S-phase factors, and lymph node metastases. Increased EGF reception may be associated with worse relapse free and survival time.
p53 Gene—used to predict prognosis. This tumor suppressor gene regulates cell cycles. Some clinicians believe that the prognostic value of the p53 gene is second only to lymph node status.
c-erbB2 (HER2) oncogene—determines which patients are most likely to benefit from high doses of chemotherapy. High levels of this oncogene receptor are associated with poor response to conventional chemotherapy and may be a marker for patients likely to benefit from high doses of chemotherapy. HER2/neu levels may also be determined in a blood specimen.
See Chapter 10 for image-guided tumor localization study before biopsy.
Breast tissue specimens may be obtained by open surgical technique, x-ray-guided core biopsy, needle biopsy, or MRI-guided biopsy.
MRI-guided breast biopsy is performed by positioning the patient with both breasts in a dedicated surface breast coil. The breast to be biopsied is positioned in a compression device, and a marker
(vitamin E capsule) is taped over the suspected area of the lesion. Subsequently, an intravenous (IV) injection of gadopentetate dimeglumine is given, and images are acquired after contrast injection. This process is used to determine the depth and location of the lesion for insertion of a probe. A needle can now be introduced and a small, cylindrical tissue sample obtained. The procedure generally takes less than 60 minutes.
Place these specimens in a biohazard bag, take directly to the laboratory, and give to the pathologist or histotechnologist. The breast tissue is examined and the extent of the tumor determined. Reaction margins and the grade and stage of disease are identified.
See Chapter 1 guidelines for intratest care.
 PROCEDURAL ALERT
PROCEDURAL ALERT
After breast tissue is examined, the extent of the tumor is determined. Resection margins are evaluated, and grade and stage of disease are identified. The further dedifferentiated a tumor becomes, the further it deviates from the normal diploid state. This may be expressed as a tetraploid or aneuploid state according to the amount of DNA on the stained tissue (DNA index of between 1.0 and 2.0). The more cells in the S or DNA phase, the more aggressive the tumor.
Favorable prognostic indicators include tumor size <1 cm, a low histologic grade, negative axillary lymph nodes, and positive ER and PR.
Fibroplasia and fibroadenoplasia are benign conditions.
Explain biopsy purpose and procedure. Obtain and record relevant family or personal history of prior biopsy, trauma, recent or current pregnancy, nipple discharge, location of lump, and how lesion was detected. Obtain informed consent.
Be aware that open breast biopsies are performed under local or general anesthesia. Sedation may be used with local anesthetics. NPO is required when general anesthesia is used.
Provide information and support, recognizing the fear the patient experiences about the procedure.
See Chapter 1 guidelines for safe, effective, informed pretest care.
If general anesthesia is used, follow the recovery protocols.
Interpret biopsy outcome and counsel appropriately about possible further testing and treatment (surgery, radiation, and medication [chemotherapy]).
See Chapter 1 guidelines for safe, effective, informed posttest care.
computes a Gail Index Score in a woman of a given age and with the presence of certain factors that indicate risk for developing breast cancer over a specified interval. The Gail Index Score is based on risk factors (e,g., late age at menarche, late age at first live birth, number of previous biopsies, and number of first-degree relatives with breast cancer).
Apply a local anesthetic cream to the nipple area using a special kit; use a suction device to draw tiny amounts of fluid droplets from the milk ducts to the nipple surface. These droplets locate the milk ducts’ natural opening on the surface of the nipple.
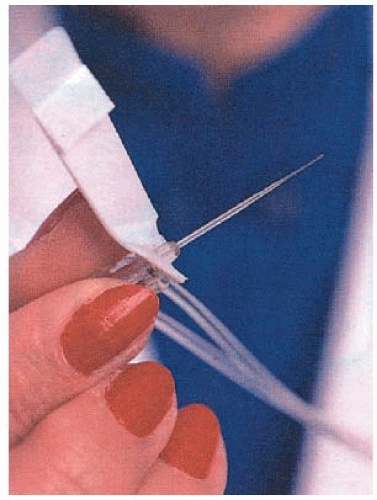
Insert a very fine (hair-thin) catheter (Fig. 11.1) into the periareolar duct. Administer local anesthetic into the duct. Use a saline wash to separate the cells. Place the specimen in a special collector vial and send for examination in a biohazard bag.
Abnormal findings include atypical hyperplasia and evidence of proliferative breast disease. The presence of atypical cells increases the risk for breast cancer by four to five times compared with women who do not have atypical cells.
Relative risk is increased even further in the presence of a family history of breast cancer (mother, daughter, sister, or two or more close relatives with history of breast cancer), specific genetic change (BRCA-1 and BRCA-2 mutations), and a Gail Index Score of at least 1.7.
The age-specific composite evidence rate of the Gail Model increases rapidly with age, although the conversion model changes little with age.
Later relative risk (%) or estimate of developing breast cancer within 10, 20, or 30 years of follow-up is based on projected probability.
Explain the lavage purpose, procedure, benefits, and risks.
Be aware that high-risk women of any age may be good candidates for ductal lavage. Obtain appropriate history of risk.
Describe sensations that might be felt: feelings of fullness, pinching, and gentle tugging on the breast, which is uncomfortable, but not usually painful.
See Chapter 1 guidelines for safe, effective, informed pretest care.
Interpret test results and counsel appropriately about chance of breast cancer development, followup, close monitoring (yearly examinations), and preventive drug treatment (e.g., tamoxifen) or surgery (oophorectomy or bilateral mastectomy).
Remember that test outcomes are interpreted in conjunction with mammogram and physical examination findings.
See Chapter 1 guidelines for safe, effective, informed posttest care.
Be aware that in most cases, this is an outpatient procedure.
Remember that the test may be done at the bedside in a special area, usually under local anesthesia. Obtain specimens with ultrasound or computed tomography (CT) x-ray guidance and a tissue core biopsy needle, such as the Menghini needle, that provides histologic and cytologic material; or use a fine-needle aspiration needle, which obtains cytologic material only and is useful for cancer diagnosis but not diagnosis of other liver diseases. It is done from an anterior approach.
Place tissue specimens in 10% formalin for fixation. Do not place specimens for culture in a fixative. Check with your laboratory for specific instructions for handling special cases (e.g., liver biopsies for copper levels).
Express cytology specimens on glass slides and fix immediately in 95% alcohol. Needle rinses may provide helpful diagnostic material as well.
See Chapter 1 for safe, effective, informed intratest care. See Chapter 12 on endoscopic examination and liver biopsy.
Benign disorders, such as those causing liver cirrhosis, and presence of pathogenic organisms in liver abscess
Metabolic disorders:
Fatty metamorphosis
Hemosiderosis
Accumulation of bile (hepatitis, obstructive jaundice, malignancy)
Diabetic pathology and Wilson’s disease (tissue copper is elevated per dry tissue weight)
Hepatic cysts (congenital or hydatid)
Malignant processes such as end stage of lymphomas
False-negative results may be caused by:
Sampling error. Detection rate of liver metastases is approximately 50% to 70% with blind biopsy and about 85% (range, 67% to 96%) with the use of ultrasound guidance. Also, many diseases produce nonspecific changes that may be spotty, healing, or minimal.
Degeneration or distortion caused by faulty preparation of specimen.
False-positive results may be caused by misinterpretation of markedly reactive hepatocytes.
Explain the purpose, procedure, benefits, and risks of the test. Obtain properly signed, informed consent. The procedure usually causes minimal discomfort, but only for a short while. Explain that a local anesthetic will be injected into the skin. Remember to ask whether the patient has ever had a reaction to any numbing medicines. Discontinue all aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) for at least 7 days before the procedure. Prothrombin time (PT), partial thromboplastin time (PTT), blood urea nitrogen (BUN), bleeding time, and type L screen cross-match for possible transfusion are usually ordered before biopsy.
Ensure that the patient takes nothing by mouth (non per os, NPO) for 4 to 6 hours before the procedure. Ask the patient to lie supine with the right arm above the head. During the biopsy, the patient should take a deep breath in, blow the air out, and then hold the breath.
Be aware that risks include a small but definite risk for intra-abdominal bleeding and bile peritonitis. Percutaneous liver biopsy results in complications in only about 1% of cases.
See guidelines in Chapter 1 for safe, effective, informed pretest care.
Bleeding diathesis—anticoagulant therapy
Highly vascular lesions
Uncooperative patient
PT in the anticoagulant range; PTT more than 20 seconds over control
Severe anemia (hemoglobin <9.5 g/dL or <95 g/L) or marked prolonged bleeding time
Infection
Platelet count >50,000/mm3 (50 × 109/L)
Marked or tense ascites (risk for leakage)
Septic cholangitis
Remember that strict bed rest for at least 6 hours is usually ordered, with observation for 24 hours.
Monitor in a recovery area. Assess pulse, blood pressure, and respiration every 15 minutes for the first hour, every 30 minutes for the next 2 hours, once in each of the next 4 hours, and then every 4 hours until the patient’s condition is stable.
Notify the surgeon if the blood pressure differs markedly from baseline or if the patient is in severe pain.
Maintain NPO status for 2 hours; previous diet can then be resumed. Take action immediately if a bleeding episode occurs. Assess for pain and treat as ordered.
After 6 hours, a blood specimen for hematocrit testing is usually ordered to rule out internal bleeding. A small number of patients need transfusion for intraperitoneal bleeding.
Warn the patient not to cough hard or strain for 2 to 4 hours after the procedure. Heavy lifting and strenuous activities should be avoided for about 1 week.
The most common complications include uncontrolled pain, hemorrhage (cause of death from liver biopsy), peritonitis, bile leakage, lacerations of other organs, sepsis, and bacteremia.
Follow the guidelines in Chapter 1 for safe, effective, informed posttest care.
Obtain a specimen of kidney tissue (containing 8 to 10 glomeruli) by needle biopsy or open surgical technique using x-ray or ultrasound as a guide.
Place in normal saline until frozen or place in a fixative or saline and send immediately to the laboratory. Check with your laboratory for specific handling instructions. Proper handling is critical to ensure that the specimen is properly preserved for necessary testing.
See Fine-Needle Aspirates: Cell (Cytologic) and Tissue (Histologic) Study for information regarding obtaining kidney material for cytologic study.
Explain purpose, procedure, benefits, and risks of kidney biopsy.
Use sedation and local or general anesthesia if necessary.
Obtain signed, witnessed consent.
Be aware that contraindications include uncontrolled bleeding, cancer, large cysts, abscess, pregnancy, acute pyelonephritis, aneurysm, and renal artery.
In counsel with other clinicians, counsel patient and interpret test outcomes, discussing further testing and possible treatment.
Monitor for complications, which include hematuria (more common in uncontrolled hypertension and uremia), hematomas (presence of a local mass), infection, and laceration of other organs.
Procedure for obtaining sputum
Be aware that the preferred material is an early-morning specimen. Usually, three specimens are collected on 3 separate days.
Have the patient inhale air to the full capacity of the lungs and then exhale the air with an expulsive deep cough.
Have the patient cough the specimen directly into a wide-mouthed, clean container containing 50% alcohol. (Some cytology laboratories prefer the specimen to be fresh if it will be delivered
to the laboratory immediately.) If microbiologic studies are also ordered, the container must be sterile, and no fixative should be added.
Cover the specimen with a tight-fitting, clean lid.
Label the specimen with the patient’s name, age, date, diagnosis, and number of specimens (one, two, or three) and send immediately to the laboratory.
Procedure for obtaining bronchial secretions
Obtain bronchial secretions during bronchoscopy (see Chapter 12). Diagnostic bronchoscopy involves removal of bronchial secretions and tissue for cytologic and microbiologic studies.
Collect secretions obtained in a clean container and take to the cytology laboratory. If microbiologic studies are ordered, the container must be sterile.
Procedure for obtaining bronchial brushings
Obtain bronchial brushings during bronchoscopy.
Smear the material collected directly on all-frosted slides and immediately fix, or place the actual brush in a container of 50% ethyl alcohol or saline and deliver to the cytology laboratory (check with the laboratory for their preference).
Procedures for bronchopulmonary lavage
Use bronchopulmonary lavage to evaluate patients with interstitial lung disease.
Inject saline into the distal portions of the lung and aspirate back through the bronchoscope into a specimen container. This essentially “washes out” the alveoli.
Take the fresh specimen directly to the laboratory. A total cell count and a differential cell count are performed to determine the relative numbers of macrophages, neutrophils, and lymphocytes.
For all procedures, see Chapter 1 guidelines for intratest care.
Benign atypical changes in sputum, as in:
Inflammatory diseases
Asthma (Curschmann’s spirals and eosinophils may be found, but they are not diagnostic of the disease.)
Lipid pneumonia (Lipophages may be found, but they are not diagnostic of the disease.)
Asbestosis (ferruginous or asbestos bodies)
Viral diseases
Benign diseases of lung, such as bronchiectasis, atelectasis, emphysema, and pulmonary infarcts
Metaplasia (the substitution of one adult cell type for another); severe metaplastic changes are found in patients with:
History of chronic cigarette smoking
Pneumonitis
Pulmonary infarcts
Bronchiectasis
Healing abscess
Tuberculosis
Emphysema (Metaplasia often adjoins a carcinoma or a carcinoma in situ.)
Viral changes and the presence of virocytes (viral inclusions) may be seen in:
Viral pneumonia
Acute respiratory disease caused by adenovirus
Herpes simplex
Measles
Cytomegalic inclusion disease
Varicella
Degenerative changes, as seen in viral diseases of the lung
Fungal and parasitic diseases (In parasitic diseases, ova or parasite may be seen.)
Tumors (benign and malignant)
False-negative results may be caused by:
Delays in preparation of the specimen, causing a deterioration of tumor cells
Sampling error (Diagnostic cells may not have exfoliated into the material examined.)
The frequency of false-negative results is about 15%, in contrast to about 1% in studies for cervical cancer. This high incidence occurs even with careful examination of multiple deep cough specimens.
Mild sedative and analgesia and/or local anesthetic may be used during bronchoscopy. Analgesia is indicated for pain after bronchoscopy. See Chapter 12 for bronchoscopy care.
Sputum specimens are collected in a wide-mouthed container; 50% alcohol may be added if transportation to the laboratory will be delayed.
Bronchial washings may be collected in a trap tube or wide-mouthed container.
Bronchial brushes may be smeared directly on glass slides, which are then fixed immediately in 95% alcohol or spray fixative. Brushes may be placed in a fixative solution such as 50% alcohol.
Explain the purpose and procedure of the test. Tell the patient not to drink fixative liquid in specimen container.
Emphasize that sputum is not saliva. If a patient is having difficulty producing sputum, a hot shower before obtaining a specimen may improve the yield.
Advise the patient to brush the teeth and rinse the mouth well before obtaining the sputum specimen to avoid introduction of saliva into the specimen. The specimen should be collected before the patient eats breakfast.
If bronchoscopy is performed, maintain NPO for 6 hours before the procedure.
Manage pain with sedation as indicated.
Provide emotional support.
Instruct the patient to breathe in and out of the nose with the mouth open during the procedure. The fiberoptic bronchoscope is inserted through the nose or mouth; the rigid bronchoscope is inserted through the mouth.
See Chapter 1 guidelines for safe, effective, informed pretest care.
If the specimen is obtained by bronchoscopy, check the patient’s blood pressure and respirations every 15 minutes for 1 hour, then every 2 hours for 4 hours, then as ordered.
Assist and teach the patient to not eat or drink until the gag reflex returns.
Maintain bed rest and elevate the head of the bed 45°.
Manage pain as indicated.
Auscultate the chest for breath sounds every 2 to 4 hours and then as ordered.
Perform postural drainage and oropharyngeal suctioning as ordered. (Refer to bronchoscopy care in Chapter 12.)
Follow guidelines in Chapter 1 for safe, effective, informed posttest care.
Interpret test outcomes and provide support for abnormal outcomes.
Give a sedative before the procedure. For esophageal studies, pass a nasogastric Levin tube approximately 40 cm (to the cardioesophageal junction) with the patient in a sitting position.
For stomach studies, pass a Levin tube into the stomach (approximately 60 cm) with the patient in a sitting position.
For pancreatic and gallbladder drainage, pass a special double-lumen gastric tube orally 45 cm, with the patient in a sitting position. Then place the patient on his or her side and pass the tube slowly 8.5 cm. It takes about 20 minutes for the tube to reach this distance. Confirm the tube location by biopsy. Lavage with physiologic salt solution is done during all upper gastrointestinal cytology procedures.
Be aware that specimens can also be obtained during endoscopy procedures.
Remember that material obtained with the use of brushes may be smeared directly on glass slides, which are fixed immediately in 95% alcohol or spray fixative. Brushes may also be placed in a fixative such as 50% alcohol. See Chapter 12 for endoscopic biopsy procedures. Washings must be delivered immediately to the laboratory and may need to be placed on ice. Check with your individual laboratory for specific instructions on handling of washings from the gastrointestinal tract.
The characteristics of benign and malignant cells of the gastrointestinal tract are the same as for cells of the rest of the body.
Abnormal results in cytologic studies of the esophagus may be a nonspecific aid in the diagnosis of:
Acute esophagitis, characterized by increased exfoliation of basal cells with inflammatory cells and polymorphonuclear leukocytes in the cytoplasm of the benign squamous cells
Vitamin B12 and folic acid deficiencies, characterized by giant epithelial cells
Malignant diseases, characterized by typical cells of esophageal malignancy
Abnormal results in studies of the stomach may be a nonspecific aid in the diagnosis of:
Pernicious anemia, characterized by giant epithelial cells. An injection of vitamin B12 causes these cells to disappear within 24 hours.
Granulomatous inflammations seen in chronic gastritis and sarcoidosis of the stomach, which is characterized by granulomatous cells
Gastritis, characterized by degenerative changes and an increase in the exfoliation of clusters of surface epithelial cells
Malignant diseases, most of which are gastric adenocarcinomas. Lymphoma cells can be differentiated from adenocarcinoma. The Reed-Sternberg cell, a multinucleated giant cell, is the characteristic cell found along with abnormal lymphocytes in Hodgkin’s disease.
Abnormal results in studies of the pancreas, gallbladder, and duodenum may reveal malignant cells (usually adenocarcinoma), but it is sometimes difficult to determine the exact site of the tumor.
Abnormal results in examination of the colon may reveal:
Ileitis, characterized by large, multinucleated histocytes (Bovine tuberculosis commonly manifests itself in this area.)
Ulcerative colitis, characterized by hyperchromatic nuclei surrounded by a thin cytoplasmic rim
Malignant cells (usually adenocarcinoma)
Tell the patient the purpose of this test, the nature of the procedure, and to anticipate some discomfort.
Be aware that a liquid diet usually is ordered for the 24 hours before testing. Encourage the patient to take fluids throughout the night and in the morning before the procedure.
Do not administer oral barium for the preceding 24 hours.
Remember that laxatives and enemas are ordered for colon cytologic studies.
Because insertion of the nasogastric tube can cause considerable discomfort, devise a system (e.g., raising a hand) with the patient to indicate discomfort. (See gastric analysis procedure in Chapter 16.)
Inform the patient that panting, mouth breathing, or swallowing can help to ease insertion of the tube.
Tell the patient that sucking on ice chips or sipping through a straw also makes insertion of the tube easier.
Remember that ballottement and massage of the abdomen are needed to release cells when a gastric wash technique is used.
See Chapter 1 guidelines for safe, effective, informed pretest care.
The uncooperative patient is a contraindication.
Immediately remove the tube if the patient shows signs of distress: coughing, gasping, or cyanosis.
Interpret test results and monitor appropriately. The patient should be given food, fluids, and rest after the tests are completed.
Provide rest. Patients having colon studies will be feeling quite tired.
Be aware that potential complications of endoscopy include respiratory distress and esophageal, gastric, or duodenal perforation. Complications of proctosigmoidoscopy include possible bowel perforation. Decreased blood pressure, pallor, diaphoresis, and bradycardia are signs of vasovagal stimulation and require immediate notification of the physician.
Follow Chapter 1 guidelines for safe, effective, informed posttest care.
Superficial squamous cells (mature squamous, usually polygonal, containing a pyknotic [thick, compact, dense] nucleus)
Intermediate squamous cells (mature squamous, usually polygonal, containing a clearly structured vesicular nucleus, which may be either well preserved or changed as a result of bacterial cytolysis)
Parabasal cells (immature squamous, usually round or oval, containing one or, rarely, more than one) as a result of degeneration or necrosis
Cytologic findings alone do not form the basis for a diagnosis of cancer or other diseases. Often, they are used to justify further procedures, such as biopsy.
The Pap smear has been approved by the U.S. Food and Drug Administration (FDA) for diagnosis of cancer and HPV.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree