Colonoscopy
Colonoscopy is performed with the patient lying in the left lateral decubitus (Sims) position. Flexible sigmoidoscopy will not be discussed separately because it duplicates the initial maneuvers of colonoscopy. Concentrate on passing the scope safely and atraumatically. Inspect the region as the scope is withdrawn. Use as little air insufflation as possible to ensure patient comfort and to facilitate passage of the scope. This procedure is used to introduce the topography of the colon.
Steps in Procedure
Assure intravenous access and provide sedation, if desired
Position patient in left lateral decubitus position
Perform digital rectal examination
Pass lubricated colonoscope past anal sphincters
Pass Scope Under Direct Vision to Cecum
Use as little insufflation as possible
The rectum hugs the curve of the sacrum and has three prominent valves
At the pelvic brim, angulation marks the entry into the mobile sigmoid colon
The next angulation is encountered at the splenic flexure
The three haustra of the transverse colon usually give it a triangular cross-section
The next angulation is the hepatic flexure (sometimes aspirating some air helps)
The cecum shows convergence of taeniae, appendiceal orifice and ileocecal valve may be seen
Inspect the entire bowel as you slowly withdraw the scope
Hallmark Anatomic Complications
Missed lesions due to blind spots
Perforation
List of Structures
Rectum
Transverse rectal folds (valves of Houston)
Sigmoid colon
Descending (left) colon
Splenic flexure
Transverse colon
Hepatic flexure
Ascending (right) colon
Cecum
Ileocecal valve
Rectosigmoid (Fig. 78.1)
Technical Points
Perform a digital rectal examination first to lubricate the anal canal and to confirm that no low obstructing lesions are present. If stool is encountered, consider rescheduling the examination after completion of a more adequate bowel prep.
Place the index finger of your dominant hand on the tip of the scope and press the tip, angled at about 45 degrees, against the anus. Instruct the patient to bear down. This will relax the sphincters and facilitate passage of the scope. Press the scope into the anal canal. Note that the rim of the scope is elevated, which makes insertion of the tip en face difficult, if not impossible.
The rectum curves posteriorly to hug the hollow of the sacrum. Insufflate enough air to identify its lumen. The valves of Houston may be visible.
At the pelvic brim, the relatively straight rectum blends imperceptibly with the mobile sigmoid. The length and mobility of this segment vary considerably from individual to individual and may be altered by prior surgery. Try to traverse the sigmoid using as little length of the scope and as little air insufflation as possible.
Anatomic Points
Flexible endoscopy has significantly decreased the incidence of perforation of the rectum. However, because perforations still occur, one should be aware of the anatomy and relationships
of the rectum and anal canal. As the terminal rectum penetrates the pelvic diaphragm, it makes an approximate right-angled bend. From the standpoint of the endoscopist inserting an instrument into the anus, this bend occurs about 4 cm proximal to the anal verge (here defined as the transition zone where the dry, hirsute, perianal skin changes to the moist, squamous epithelium lining the anal canal). This necessitates directing the tip of the instrument toward the concavity of the sacrum. Immediately anterior to this point of angulation are the median prostate gland and paramedian seminal vesicle in male patients, and the vagina in female patients. In male patients, more proximally, the anterior rectal wall is in contact with the urinary bladder. Still further from the anal verge (about 7.5 cm in males and 5.5 cm in females), the peritoneum is reflected from the anterior surface of the rectum to the posterior surface of the urinary bladder (in males) or the uterus (in females), forming the rectovesical or rectouterine pouch (cul-de-sac of Douglas), respectively. This is the most dependent recess of the peritoneal cavity; thus, it can fill with peritoneal fluid, pus, or loops of bowel.
of the rectum and anal canal. As the terminal rectum penetrates the pelvic diaphragm, it makes an approximate right-angled bend. From the standpoint of the endoscopist inserting an instrument into the anus, this bend occurs about 4 cm proximal to the anal verge (here defined as the transition zone where the dry, hirsute, perianal skin changes to the moist, squamous epithelium lining the anal canal). This necessitates directing the tip of the instrument toward the concavity of the sacrum. Immediately anterior to this point of angulation are the median prostate gland and paramedian seminal vesicle in male patients, and the vagina in female patients. In male patients, more proximally, the anterior rectal wall is in contact with the urinary bladder. Still further from the anal verge (about 7.5 cm in males and 5.5 cm in females), the peritoneum is reflected from the anterior surface of the rectum to the posterior surface of the urinary bladder (in males) or the uterus (in females), forming the rectovesical or rectouterine pouch (cul-de-sac of Douglas), respectively. This is the most dependent recess of the peritoneal cavity; thus, it can fill with peritoneal fluid, pus, or loops of bowel.
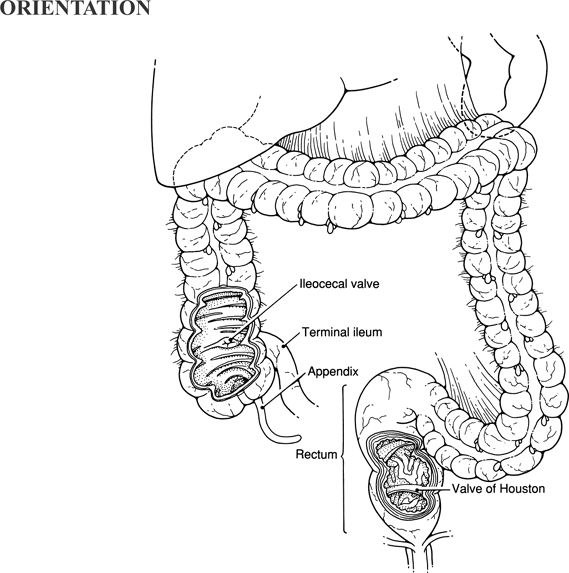 |
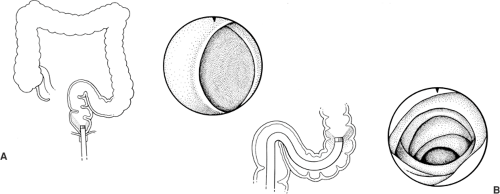 Figure 78-1 Rectosigmoid
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|