Chronic Neutrophilic Leukemia
Kaaren K. Reichard, MD
Key Facts
Terminology
Chronic neutrophilic leukemia (CNL)
Etiology/Pathogenesis
Unknown
Extremely rare disease
Clinical Issues
Hepatosplenomegaly
Bleeding, gout, pruritus
Microscopic Pathology
PB neutrophilia; blasts < 1%, WBC ≥ 25 × 109/L, immature granulocytes < 10% of WBC
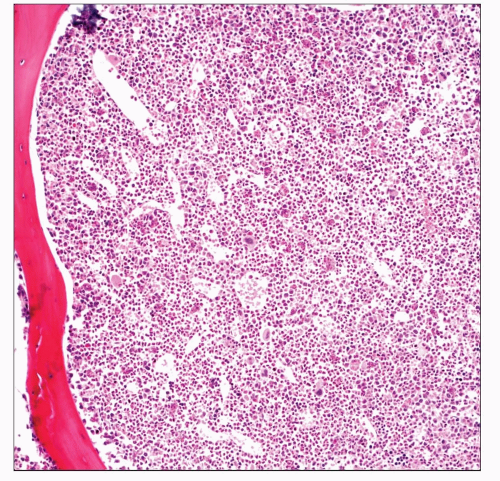
BM hypercellular with granulocytic predominance; blasts < 5%, occasional erythroid and megakaryocytic proliferation
No dysplasia, overt basophilia, or monocytosis
Ancillary Tests
Genetics
Absence of BCR-ABL1 fusion
No rearrangement of PDGFRA, PDGFRB, and FGFR1
Cytogenetics most often normal
JAK2 V617F mutation has been reported
Top Differential Diagnoses
Reactive neutrophilia
Infection, inflammation, collagen vascular disease, underlying neoplasm
Myeloma may lead to “CNL-like” picture
CML, BCR-ABL1 positive
Particularly neutrophilic variant
p230 variant of BCR-ABL1 fusion
BCR-ABL1 negative MPNs
Survival ranges from < 1 year to > 20 years
Median survival < 2 years
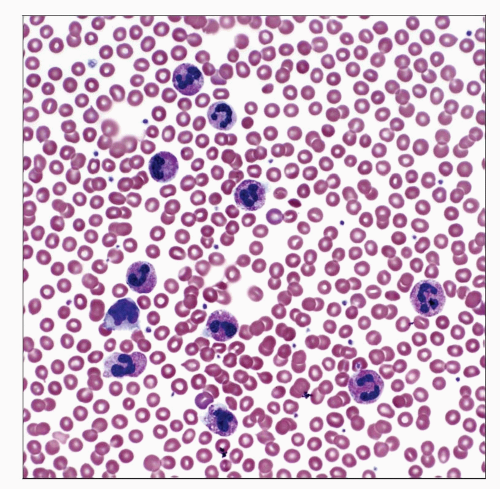 This peripheral blood smear demonstrates the typical neutrophilic leukocytosis with minimal left shift in a case of chronic neutrophilic leukemia. |
TERMINOLOGY
Abbreviations
Chronic neutrophilic leukemia (CNL)
Definitions
Clonal hematopoietic neoplasm manifesting predominantly in granulocytic lineage
Persistent peripheral blood (PB) neutrophilia
Persistent bone marrow (BM) granulocytic proliferation
Reactive neutrophilia and other myeloproliferative neoplasms (MPNs) must be completely excluded
BCR-ABL1 negative
ETIOLOGY/PATHOGENESIS
Unknown
Rare disease
< 500 cases reported in the literature
CNL neutrophils may be dysfunctional
Decreased stimulation with granulocyte colony stimulating factor (G-CSF)
Insufficiency of some inflammatory cytokinespecific signaling
CLINICAL ISSUES
Epidemiology
Age
Median: 6th decade
Gender
Slight male predominance
Presentation
Abnormal complete blood cell count (CBC)
Hepatomegaly
Splenomegaly
Neutrophilia
Majority of patients asymptomatic
Gout
Pruritus
Mucocutaneous bleeding
Laboratory Tests
CBC
PB and BM examination
Cytogenetics
Treatment
Variable
Depends on symptomatology
Watchful waiting
If indolent
Cytoreductive agents (e.g., hydroxyurea)
Toxic chemotherapy
If progressive or symptomatic disease
Allogeneic stem cell transplant in rare cases
Progressive disease
Development of myelodysplasia or acute leukemia
Unclear, in some cases, if result of prior toxic treatment
Prognosis
Heterogeneous
May be indolent
Disease progression
Progressive neutrophilia refractory to therapy
Progressive splenomegaly
Refractory thrombocytopenia with bleeding complications
Cytogenetic clonal evolution
Myelodysplasia may develop
Rare leukemic transformation
Death from
Intracranial hemorrhage
Infection
Bone marrow failure
IMAGE FINDINGS
Radiographic Findings
Hepatomegaly
Splenomegaly
MICROSCOPIC PATHOLOGY
Peripheral Blood
Neutrophilia and increased band forms
WBC ≥ 25 × 109/L
Toxic changes with prominent granules may be seen
Must exclude reactive condition
Absence of dysplasia
No significant basophilia
No significant monocytosis
Immature granulocytes (metamyelocytes, myelocytes, and promyelocytes) constitute < 10% of WBC
Blasts comprise < 1% of WBC
Variable anemia and thrombocytopenia
Erythrocytes and platelets morphologically normal
Bone Marrow
Hypercellular; granulocytic predominance; blasts < 5%
May see megakaryocytic &/or erythroid proliferation
May see histiocytic neutrophilic phagocytosis
No dysplasia
No significant reticulin fibrosis
Normal bony trabeculae
Ancillary Studies
Conventional cytogenetics
90% of cases are cytogenetically normal
Reported abnormalities include +8, +9, +21, and del(20q)
Clonal evolution with disease progression
Absence of recurrent genetic abnormality defining another myeloid disorder
t(9;22)(q34;q11.2) in chronic myelogenous leukemia
Rearrangements of PDGFRA, PDGFRB, and FGFR1
Fluorescence in situ hybridization
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree