Cervical Lymph Node Biopsy and Scalene Node Biopsy
Lymph node biopsy is only very rarely performed now for diagnostic purposes. Cervical lymph node biopsy should only be performed when a careful examination of the aerodigestive tract has failed to demonstrate a primary carcinoma and other means of diagnosis have failed. Biopsy of a cervical lymph node that is found to contain metastatic carcinoma from a head and neck primary tumor is a grave error because such biopsy contaminates the field should subsequent radical neck dissection be contemplated. For this reason, open surgical biopsy has largely been supplanted by fine-needle aspiration cytology. Open surgical biopsy is rarely indicated.
For optimum histologic classification of lymphomas, an entire lymph node with its capsule may be needed. Thus, the goal of diagnostic lymph node biopsy is to remove the node intact with minimal trauma.
Scalene node biopsy is performed by removing the fatty node-bearing tissue in the scalene triangle. Formerly performed for diagnosis and staging of lung cancer, it is now occasionally used for other malignancies.
Cervical lymph node biopsy and the closely related scalene node biopsy are discussed in this section, and the major cervical lymph node groups are presented. The anatomy of this region is described in greater detail in Chapter 11.
SCORE™, the Surgical Council on Resident Education, does not list cervical or scalene node biopsy; it does, however, classify excisional and incisional biopsy of soft tissue lesions as an “ESSENTIAL COMMON” procedure. That procedure requires the skills described in the current chapter.
STEPS IN PROCEDURE
Transverse skin crease incision over node of interest
Deepen through platysma
Retract sternocleidomastoid muscle if necessary to expose node
Remove node, ligating hilum
HALLMARK ANATOMIC COMPLICATIONS
Compromise future radical neck dissection field
Injury to thoracic duct (left side)
LIST OF STRUCTURES
Platysma muscle
Sternocleidomastoid muscle
Omohyoid muscle
Anterior scalene muscle
Carotid sheath
Thoracic duct
Phrenic nerve
Thyrocervical trunk
Cervical lymph nodes
Scalene lymph nodes
Major Lymph Node Groups of the Neck (Fig. 10.1)
Technical Points
Lymph nodes are clustered in regions where major vessels converge. In the head and neck, the nodes most commonly selected for biopsy follow the internal jugular vein.
Anatomic Points
Although the position of lymph nodes and the groups of lymph nodes in the neck are relatively constant, the terminology applied to these nodes is not. Here, we follow the terminology of Terminologia Anatomica (Fig. 10.1A) and compare it with that used for cancer staging as described in the American Joint Committee on Cancer Staging Manual (Fig. 10.1B).
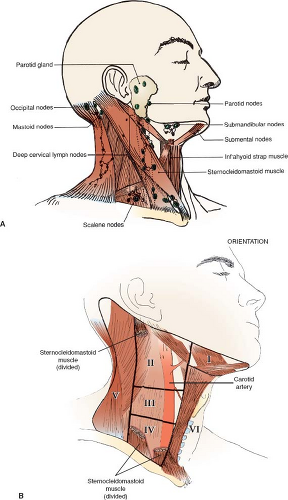 Figure 10.1 Major lymph node groups of the neck. A: Terminologia anatomica; B: Cervical lymph node biopsy. |
In general, lymph node groups in the neck can be considered to form a pericraniocervical ring (essentially at the head–neck junction), superficial and deep vertical chains, and perivisceral deep nodes. Lymph node groups in the pericraniocervical ring receive afferent lymph vessels from adjacent head regions or from other groups in the ring. The vertical cervical chains, in addition to receiving afferent lymph vessels from nodes in the pericraniocervical ring, also receive afferents directly from the cranial regions (lymph thus “skips” the immediate regional nodes) and from perivisceral nodes in the neck. The following is a list of most of the regional lymph nodes and what these groups of nodes drain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


