To examine the spinal fluid for diagnosis of four major disease categories:
Meningitis
Subarachnoid hemorrhage
CNS malignancy (meningeal carcinoma, tumor metastasis)
Autoimmune disease and multiple sclerosis
To determine level of CSF pressure, to document impaired CSF flow, or to lower pressure by removing volume of fluid (fluid removal should be done with caution)
TABLE 5.1 Normal CSF Values
Volume
Appearance
Pressure
Total cell count
Adult: 90-150 mL; child: 60-100 mL
Crystal clear, colorless
Adult: 90-180 mm H2O; child: 10-100 mm H2O
Essentially free cells
Adults
Newborn (0-14 d)
WBCs
Differential
0-5 cells
0-30 cells
Lymphocytes
40%-80% (0.40-0.80)
5%-35% (0.05-0.35)
Monocytes
15%-45% (0.15-0.45)
50%-90% (0.50-0.90)
Polys
0%-6% (0-0.06)
0%-8% (0-0.08)
RBCs (has limited diagnostic value)
Specific gravity
1.006-1.008
Clinical Tests
Glucose
40-70 mg/dL (2.2-3.9 mmol/L)
60-80 mg/dL (3.3-4.4 mmol/L)
Protein
Lumbar
Adults: 15-45 mg/dL (150-450 mg/L)
Neonates: 15-100 mg/dL (150-1000 mg/L)
Elderly (>60 y): 15-60 mg/dL (150-600 mg/L)
Cisternal
15-25 mg/dL (150-250 mg/L)
Ventricular
5-15 mg/dL (50-150 mg/L)
Lactic acid (lactate)
10-24 mg/dL (1.11-2.66 mmol/L)
Glutamine
5-20 mg/dL (0.34-1.37 mmol/L)
Albumin
10-35 mg/dL (1.52-5.32 mmol/L)
Urea nitrogen
6-16 mg/dL (2.14-5.71 mmol/L)
Creatinine
0.5-1.2 mg/dL (44-106 mmol/L)
Uric acid
0.5-4.5 mg/dL (29.7-268 mmol/L)
Bilirubin
0 (none)
Phosphorus
1.2-2.0 mg/dL (387-646 mmol/L)
Ammonia
10-35 mg/dL (5.87-20.5 mmol/L)
Lactate dehydrogenase (LDH) (10% of serum level)
Adult: 0-40 U/L (0-0.67 mkat/L)
Electrolytes and pH
pH
Lumbar
7.28-7.32
Cisternal
7.32-7.34
Chloride
115-130 mEq/L (mmol/L)
Sodium
135-160 mEq/L (mmol/L)
Potassium
2.6-3.0 mEq/L (mmol/L)
CO2 content
20-25 mEq/L (mmol/L)
PCO2
44-50 mm Hg (5.8-6.6 kPa)
PO2
40-44 mm Hg (5.3-5.8 kPa)
Calcium
2.0-2.8 mEq/L (mmol/L)
1.0-1.4 mEq/L (mmol/L)
Magnesium
2.4-3.0 mEq/L (mmol/L)
1.2-1.5 mEq/L (mmol/L)
Osmolality
280-300 mOsm/kg (280-300 mmol/kg)
Serology and Microbiology
VDRL
Negative
Bacteria
None present
Viruses
None present
Antibody index
>1.5 indicates chronic inflammatory process
<0.4 probably not acute inflammatory process
Be sure to include patient’s age because it is needed to evaluate borderline values.
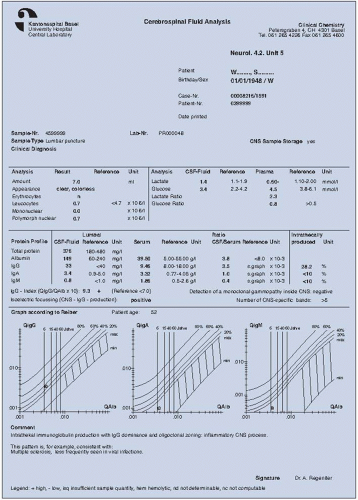
To identify disease-related immunoglobulin patterns (IgG, IgA, and IgM referenced to albumin) in neurotuberculosis, neuroborreliosis (after a tick bite), or opportunistic infections
To introduce anesthetics, drugs, or contrast media used for radiographic studies and nuclear scans into the spinal cord
To confirm the identity of pathogens involved in acute inflammatory or chronic inflammatory disorders (e.g., multiple sclerosis and blood-brain barrier dysfunction)
To identify extent of brain infarction or stroke
To formulate antibody index (AI) of the IgG class for polyspecific immune response in the central nervous system (CNS). Examples: measles, rubella, and zoster (MRZ) antibodies to viruses in multiple sclerosis (MS); herpes simplex virus (HSV) antibodies in MS; toxoplasma antibodies in MS; and autoantibodies to double-stranded deoxyribonucleic acid (ds-DNA)
To identify brain-derived proteins, such as neuron-specific enolase present after brain trauma
CSF pressure is measured.
General appearance, consistency, and tendency of the CSF to clot are noted.
CSF cell count is performed to distinguish types of cells present; this must be done within 2 hours of obtaining the CSF sample.
CSF protein and glucose concentrations are determined.
Other clinical serologic and bacteriologic tests are done when the patient’s condition warrants (e.g., culture for aerobes and anaerobes or tuberculosis).
Tumor markers may be present in CSF; these tests are useful as supplements to CSF cytology analysis (Table 5.2).
TABLE 5.2 Tumor Markers in CSF | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
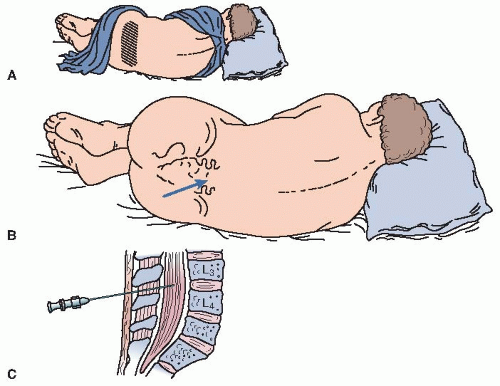
the spinal processes. However, a sitting position with the head flexed to the chest can be used. The patient is helped to relax and instructed to breathe slowly and deeply with his or her mouth open.
 PROCEDURAL ALERT
PROCEDURAL ALERT
If intracranial pressure (ICP) is elevated, especially in the presence of papilledema or split cranial sutures. However, with some cases of increased ICP, such as with a coma, intracranial bleeding, or suspected meningitis, the need to establish a diagnosis is absolutely essential and outweighs the risks of the procedure.
A relative contraindication would be ICP from a suspected mass lesion. To reduce the risk for brain herniation, a less invasive procedure such as a CT scan or magnetic resonance imaging (MRI) should be done.
Suspected epidural infection
Infection or severe dermatologic disease in the lumbar area, which may be introduced into the spinal canal
Severe psychiatric or neurotic problems
Chronic back pain
Anatomic malformations, scarring in puncture site areas, or previous spinal surgery at the site
Intracranial tumors; abscess; lesions
Meningitis (bacterial, fungal, viral, or syphilitic)
Hypo-osmolality as a result of hemodialysis
Congestive heart failure
Superior vena cava syndrome
Subarachnoid hemorrhage
Cerebral edema
Thrombosis of venous sinuses
Conditions inhibiting CSF absorption
Circulatory collapse
Severe dehydration
Hyperosmolality (increased osmotic concentration)
Leakage of spinal fluid
Spinal-subarachnoid block
Tumors or spinal blockage above the puncture site when there is a large pressure drop (no further fluid should be withdrawn)
Hydrocephalus when there is a small pressure drop that is indicative of a large CSF pool
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree