Cerebellum and Brainstem: Diagnosis
SURGICAL/CLINICAL CONSIDERATIONS
Goal of Consultation
Diagnosis to determine appropriate intraoperative and postoperative treatment
Resection (e.g., ependymoma)
Biopsy for diagnosis followed by treatment with radiotherapy or chemotherapy (e.g., medulloblastoma)
Proper handling of tissue for ancillary studies (i.e., molecular studies, electron microscopy, microbiologic culture)
Change in Patient Management
Immediate intraoperative planning, as well as diagnostic tissue allocation
Clinical Setting
3 main clinical scenarios requiring tissue sampling
Patients with symptoms and signs of increased intracranial pressure, such as nausea and vomiting
Urgent surgery to prevent impending herniation
Patients with chronic or subacute symptoms, such as ataxia and seizures
Biopsy to diagnose a slow-growing or insidious process
Patients with specific cranial nerve palsies or hearing loss
Indicative of subarachnoid involvement by inflammatory or metastatic infiltrates or local pressure by mass lesions such as vestibular schwannomas
Biopsy to diagnose disease process
Neuroimaging
Review of imaging studies is important to determine most likely differential diagnosis for a lesion
Neuroanatomic localization
Cerebellar hemisphere: Pilocytic astrocytomas in children, metastases and hemangioblastomas in adults
Cerebellar midline: Medulloblastomas in children
4th ventricle: Ependymomas in children, subependymomas in adults
Cerebellopontine angle: Choroid plexus tumors and ependymomas in children, vestibular schwannomas and meningiomas in adults
Signal characteristics
Cysts with mural nodules in pilocytic astrocytomas, hemangioblastomas
Contrast enhancement in pilocytic astrocytomas and medulloblastomas (heterogeneous), metastases, and abscesses (rim pattern)
Decreased diffusion in infarcts, hemorrhages
Ill-defined, nonenhancing hemispheric lesions in low-grade gliomas
Rim enhancing after contrast administration in glioblastomas, lymphomas, toxoplasmosis
SPECIMEN EVALUATION
Gross
Usually very few distinctive macroscopic features
Gliomas: Soft, gray-translucent, gelatinous texture
Pilocytic astrocytomas: Firm, rubbery, white-tan
Choroid plexus tumors: Papillary fronds, prominent vasculature
Hemangioblastomas: Vascular, hemorrhagic
Vestibular schwannomas, meningiomas: Firm, fibrous, or rubbery, gray-tan; difficult to smear
Abscesses: Purulent, sometimes with fibrous wall
Many lesions are hemorrhagic (nonspecific)
Distinguish lesional from normal for frozen section and smear preparation
Brainstem, cerebellar tissue: Soft pink-white, easily smeared as thin uniform film
Meningeal tissue: Membranous, vascular, does not smear well
White matter: Pearly white, sticky, but smears well
Metastases: Granular or mucoid, pink, gray, tan-yellow or hemorrhagic, depending on type; smears in clumps
Gliomas: Usually more gray and mucoid, smears well or in strings
Frozen Section
Important not to use entire specimen (may be only specimen received)
Do smear cytologic prep 1st
Use ˜ 1 mm of tissue from both ends of core biopsy to represent proximal and distal to lesion
Frozen method
Perch tissue to be frozen on small bead of embedding medium, do not cover with medium
If core biopsy, bisect sample longitudinally, after ends were taken for smears, and freeze 1/2
Freeze quickly with light touch of metal heat extractor or cryospray to avoid ice crystals in tissue
Step section carefully into block when making slides
In some cases, cytologic preparations only may be preferable
Small specimens, suspected infectious disease, or calcified lesions
Cytology
Smear (squash) for soft specimens, works for most samples
2 or 3 ˜ 1 mm pieces may be used to represent different sites on same slide
Touch preparation for firm/fibrous/calcified lesions
Scan entire slide, as lesions may be heterogeneous
Allocation For Special Studies
Glial tumors, some metastatic tumors (lung, colon)
Reserve frozen tissue for molecular studies
Required by some cancer centers for clinical trial eligibility
Infectious specimens
Tissue should be sent for microbiologic cultures
Sterile tissue sent directly from operating room is preferable for this purpose
MOST COMMON DIAGNOSES
Diffuse Brainstem Glioma
Frozen section
Rarely biopsied
Features of diffuse astrocytoma, ± anaplasia
Smear
Hyperchromatic, ovoid or fusiform nuclei
Fibrillary background
No Rosenthal fibers
Microvascular proliferation in anaplastic tumors
Necrosis suggests glioblastoma, unless prior radiotherapy
Difficulties
Usually extremely small samples
Pilocytic Astrocytoma
Frozen section
Dense areas with fibrillary background containing Rosenthal fibers and eosinophilic granular bodies, alternating with loose, microcystic regions
Rosenthal fibers are thick, eosinophilic twisted fibers (comprised of intermediate filaments)
Oval nuclei with occasional pleomorphism, rare or no mitoses
Frequent microvascular proliferation of no prognostic significance
Necrosis rare (suggests alternative diagnosis)
Smear
Clear bipolar cytomorphology
Network of coarse Rosenthal fibers in background and eosinophilic granular bodies
Knots of microvascular proliferation
Difficulties
If sample very small, may not have all desired features
Report as “astrocytoma with piloid features”
Medulloblastoma
Frozen section
“Small blue cell tumor” with broad regions of solid tumor
Single-cell apoptosis and geographic necrosis
High mitotic rate
Variable features
Homer Wright rosettes (classical medulloblastoma)
Connective tissue septa creating nodular pattern (desmoplastic medulloblastoma)
Large, bizarre cells with prominent nucleoli (anaplastic/large cell medulloblastoma)
Not necessary to distinguish variants intraoperatively
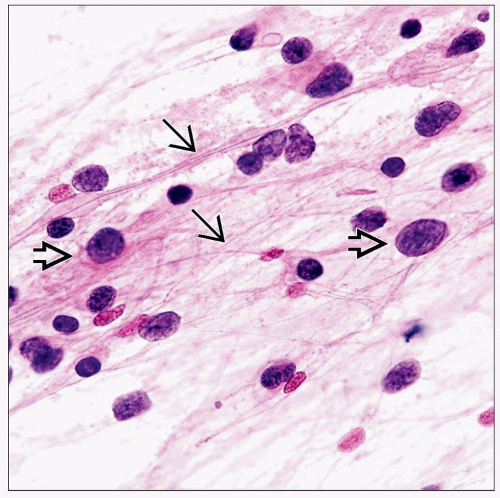
Smear
Uniform oval or carrot-shaped nuclei with little cytoplasm
Dirty necrotic background with nuclear fragments
Usually, conspicuous mitoses
Distinguish from normal cerebellar granule cells (smaller, uniformly round, bland)
Difficulties
Indistinguishable from atypical teratoid/rhabdoid tumor on intraoperative consultation
Report as “small blue cell tumor, diagnosis deferred to permanent sections”
If smear is too aggressive, nuclei may disrupt in chromatin clumps and streaks
Normal hypercellular granular cell layer of cerebellar cortex may confuse interpreter if unaware
Atypical Teratoid/Rhabdoid Tumor (AT/RT)
Frozen section
“Small blue cell tumor” without rosettes
Variably conspicuous rhabdoid cells with abundant, dense, eosinophilic cytoplasm
Occasional clear cells and “cannibal” cells (one cell engulfing another)
Smear
Predominantly uniform oval or carrot-shaped nuclei with little cytoplasm
Rhabdoid cells better seen on smear than frozen section
Nuclear debris and (usually) high mitotic rate
Difficulties
Indistinguishable from medulloblastoma on intraoperative consultation
Report as “small blue cell tumor, diagnosis deferred to permanent sections”
Ependymoma
Frozen section
Variably cellular, with perivascular pseudorosettes, ependymal tubules or canals, and small intracytoplasmic vacuoles (lumina)
Microvascular proliferation of no prognostic significance (WHO grade II)
Marked cytologic atypia, mitoses, and necrosis indicate anaplastic ependymoma (WHO grade III)
Smear
Glial tumor cells with uniform oval nuclei, often with small nucleoli and slightly granular chromatin
Cytoplasmic processes, radially arranged around blood vessels, ± vascular cell proliferation
Occasional intracytoplasmic lumina, as well as cilia and terminal bars (blepharoplasts) in tubules
Difficulties
Must establish diagnosis with reasonable certainty, as resection is definitive therapy (unlike medulloblastoma or AT/RT)
Grading may not be reliable due to tumor heterogeneity
Presence of microvascular proliferation and occasional necrosis in some grade II ependymomas
Report as “ependymoma, grading deferred to permanent sections” (unless obviously anaplastic)
Schwannoma
Frozen section
Spindle cell neoplasm with Antoni A and B areas
Antoni A areas consist of linear arrays of palisades of Schwann cell nuclei (Verocay bodies)
Antoni B areas have looser stroma and myxoid stroma
Variable nuclear size and shape, but predominantly fusiform
Hyalinized vessels, macrophages and other degenerative changes
Smear
Often tough to smear, as tissue stays in clumps; little may come off on touch prep
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree