Carotid Surgery: Distal Exposure and Control Techniques and Complication Management
Cheong J. Lee
DEFINITION
The carotid artery typically bifurcates at the level of the C3-C4 cervical spine. High carotid bifurcations and lesions that extend to the C1-C2 level pose technical challenges that may increase perioperative risk of stroke and cranial nerve injury. Ideally, the need for high access in carotid surgery should be anticipated preoperatively, with familiarity of the anatomy and exposure necessary for distal carotid control.
PATIENT HISTORY AND PHYSICAL FINDINGS
As with any medical therapy, the clinician must first clearly define the goals of treatment and thoroughly review the operative risk with the patient.
Optimal medical therapy must be instituted prior to intervention (e.g., antiplatelet agent, statin, beta-blocker).
Patients with hostile neck anatomy, such as those with history of high-dose neck radiation or severe systemic comorbidities contraindicating general or cervical block anesthesia, should be offered carotid angioplasty and stenting (CAS) as an alternative procedure.
Patients with prior contralateral carotid revascularization procedures should have laryngeal, hypoglossal, and glossopharyngeal nerve function documented prior to ipsilateral dissection and exposure. When evidence of prior injury to CN IX, X, or XII is evident, CAS should be considered as an alternative. If CAS is not feasible under these circumstances, the potential need for tracheostomy to manage postoperative airway obstruction should be reviewed with the patient.
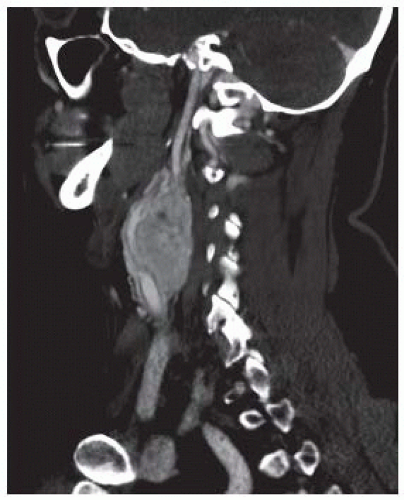
Although duplex scanning provides accurate and reproducible assessment of the presence and severity of carotid stenosis, precise anatomic detail required for surgical planning is optimally obtained from computed tomographic angiography (CTA) or magnetic resonance arteriography (MRA). Localization of the carotid bifurcation in regard to cervical landmarks, as well as the distal extent of internal carotid artery (ICA) disease, is best assessed by CTA or MRA (FIG 1).
IMAGING AND OTHER DIAGNOSTIC STUDIES
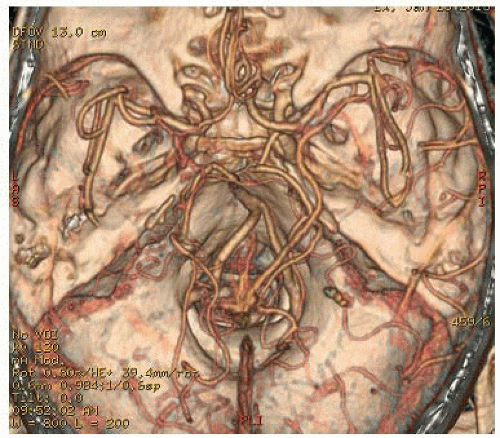
In recent years, CTA and MRA have assumed preeminent roles in carotid intervention planning. Improved resolution has enabled highly accurate characterization of plaque morphology, which may provide useful guidance regarding plaque vulnerability during operative manipulation.
MRA and CTA also provide essential information regarding potential collateral arterial flow through the circle of Willis and the need for adjuvant maneuvers such as shunt placement during carotid revascularization (FIG 2).
SURGICAL MANAGEMENT
Preoperative Planning for Distal Cervical Carotid Exposure
Knowledge of patient-specific cervical anatomy is essential to successful management of distal carotid disease. When recognized as necessary, specifying nasotracheal, rather than orotracheal, intubation for general endotracheal
anesthesia is a simple and highly effective maneuver to improve exposure. Nasotracheal intubation allows the mouth to stay closed during surgery, providing more room between the ramus of the mandible and mastoid process for distal dissection.
Temporomandibular subluxation may further advantage carotid exposure cephalad to the C2 cervical spine. Subluxation of the ipsilateral mandibular condyle, performed via intraoral wiring, facilitates exposure from infratemporal ICA to the skull base. Subluxation is distinguished from dislocation, which is more injurious and can potentiate longterm temporomandibular joint pain syndromes.
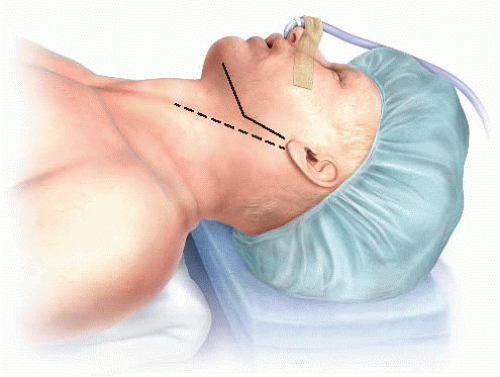
Positioning
The patient is positioned supine, with the head extended and rotated away from the operative site. Shoulder rolls and shays are placed to stabilize the neck and optimize extension. The nasotracheal tube is secured over the head (FIG 3).
Arms are tucked to the patient’s side to allow the operator and the assistant to maneuver and stand comfortably. This position also facilitates C-arm positioning when needed.
The patient is placed in the “beach chair” position to limit venous hypertension (FIG 4).
TECHNIQUES
ANTERIOR APPROACH TO THE DISTAL INTERNAL CAROTID ARTERY
Incision
A vertical, rather than transverse, cervical incision is recommended for optimal distal ICA access (FIG 5).
Standard exposure of the carotid artery in the sheath was previously described in Part 6, Chapter 3.
Exposure of the Internal Carotid Artery Distal to the Bifurcation
Key structures that lie superior to the carotid bifurcation are the posterior belly of the digastric muscle, the hypoglossal nerve, crossing veins from the sternocleidomastoid muscle to the internal jugular vein, and muscular arterioles of the posterior branches of the external carotid artery (ECA) (FIG 6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree