Carotid artery stenosis was first successfully treated via percutaneous balloon angioplasty in 1977 by Mathias and colleagues.1,2 This technique has evolved over time to include use of self-expanding nitinol stents and distal embolic protection devices (EPD). Carotid angioplasty and stenting (CAS) is indicated as an alternative to open carotid endarterectomy (CEA) in certain clinical scenarios where the patient’s anatomy and/or physiology pose a greater risk for complications with CEA. However, these specific clinical conditions are not absolute and must be weighed against risks for endovascular intervention.
Distal EPD
According to the 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease, “EPD deployment during CAS can be beneficial to reduce the risk of stroke when the risk of vascular injury is low.”3
A distal filter is placed in the internal carotid artery (ICA) distal to the lesion but below the skull base, with the purpose of capturing debris to prevent distal embolization during CAS (FIG 1). The target lesion must be crossed by the filter before deployment but this system allows for cerebral protection with maintenance of blood flow to the brain during subsequent steps of the procedure. The filter is mounted on the same wire used to perform CAS and after successful CAS, the filter is retrieved along with any captured debris.
A thorough history should be obtained prior to intervention and should include a detailed description of, if present, symptoms (quality, duration, etc.) that may be indicative of transient ischemic attacks (TIA) or prior stroke, past medical/surgical history (e.g., prior cerebrovascular disease/interventions), current medications (e.g., antiplatelet or anticoagulation medications), and social history (e.g., tobacco use).
A comprehensive physical exam is mandatory and should include a complete vascular and neurologic/stroke evaluation. Vascular exam should note the presence of palpable femoral and distal lower extremity pulses and carotid bruits.
Initial carotid duplex ultrasound is obtained to evaluate the degree of stenosis and plaque morphology. Studies have highlighted a higher potential for embolism during CAS with hypoechoic lipid-containing plaque.4
Angiographic imaging of the aortic arch and carotid and cerebral arterial vasculature must be obtained to aid in proper patient selection and procedural planning. This is accomplished through computed tomographic arteriography (CTA) (FIG 2), magnetic resonance arteriography (MRA), or catheter-based contrast arteriography.
Arch anatomy
Aortic arch morphology is variable and can change with advancing age. The arch anatomy can be divided into three types, dictated by the position of the innominate artery origin relative to two horizontal lines drawn across the apices of the outer and inner aortic arch curvatures (FIG 3).
Type I—the innominate origin arises at or above the horizontal plane of the outer arch curvature (FIG 3A) Type II—the innominate origin arises in between the two horizontal planes of the outer and inner arch curvatures (FIG 3B)
Type III—the innominate origin lies below the horizontal plane of the inner arch curvature (FIG 3C)
The difficulty in gaining access to the carotid arteries increases from types I to III. There is an increase in angle acuity of the great vessel origins off the arch with increasing arch types that make wire/catheter guidance/exchange more difficult.
Bovine arch—congenital arch variations where the left common carotid artery (CCA) shares a common origin with the innominate artery (more frequent) or the left CCA branches off the innominate artery. In a pure bovine arch (extremely rare), the right subclavian, common carotid—both right and left—and left subclavian all derive from one common arterial trunk off the aortic arch.
Shaggy aorta—when extensive aortic wall irregularities exist, there is a high risk for significant atheroembolism and thus, this may be a contraindication to CAS.
Eggshell aorta—with severe aortic wall calcification, there is increased risk of intimal disruption and difficulty of wire/catheter manipulation/advancement.
Cerebral flow to both hemispheres is assessed to determine cerebral reserve.
Carotid vessel size, tortuosity, and calcification—carotid artery diameter should be assessed to aid in determining device sizes. In addition, severe carotid circumferential calcification and vessel tortuosity may negatively impact procedural success (e.g., difficulty with inserting stent, placement of EPD in distal ICA) and may represent a contraindication to CAS.
Preoperative brain imaging with computed tomography (CT) or magnetic resonance imaging (MRI) is needed for symptomatic patients to document prior infarcts and to rule out preexisting hemorrhagic stroke prior to the initiation of the procedure.
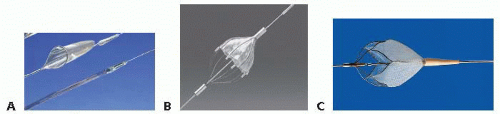 FIG 1 • Distal EPD. A. FilterWire EZ, Boston Scientific. B. Angioguard, Cordis Endovascular. C. RX Accunet, Abbot Vascular. |
The indications for any surgical intervention for carotid disease depend on the patient’s clinical status (i.e., symptomatic or asymptomatic) and the characteristics of the carotid lesion.
It has been widely accepted that appropriate candidates for CEA are symptomatic patients with carotid stenosis of 70% to 99% on noninvasive imaging and an anticipated perioperative risk of stroke or mortality of less than 6%. Benefit of intervention for symptomatic patients with lesser degrees of stenosis (50% to 69%) has also been shown but not for symptomatic patients with less than 50% carotid stenosis. CAS is an alternative to CEA for symptomatic patients meeting similar criteria along with anatomic and/or physiologic factors unfavorable for CEA (Table 1).3,5
The recommendations/indications for CAS in asymptomatic patients are still issues for debate and no consensus exists. CAS may be considered for patients with asymptomatic ICA stenosis between 70% and 99%, but there are insufficient data to recommend CAS for primary therapy in asymptomatic patients. Therefore, these patients need to be addressed on a case-by-case basis with consideration of patient comorbidities and risks of CAS.
The contraindications for CAS are predominantly related to aortic arch and carotid artery anatomic factors (Table 2).
Patients are initiated on antiplatelet therapy with aspirin 325 mg per day and clopidogrel 75 mg per day for 5 days prior to intervention. Alternatively, a clopidogrel loading dose of 300 mg can be administered 4 to 6 hours prior to the intervention.
Antihypertensive medications can be held off the day of intervention to prevent contribution to the possible periprocedural hypotension.
The patient is placed in the supine position with adequate monitoring throughout the peri- and postprocedural period. Minimal monitoring includes continuous electrocardiogram (EKG), intraarterial blood pressure, and pulse oximetry. The patient’s neurologic status must be frequently evaluated during the procedure via answering of simple questions and squeezing a plastic sound toy (e.g., rubber duck squeaky toy) in the contralateral hand.
Intraarterial blood pressure monitoring is established usually via a radial arterial line.
In order to maintain patient cooperation/comfort and frequent neurologic monitoring, minimal or no sedation is administered and only local anesthesia is infiltrated for the access site.
Table 1: Anatomic and Physiologic Factors Favoring Carotid Angioplasty and Stenting | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
Table 2: Anatomic and Physiologic Factors Unfavorable for Carotid Angioplasty and Stenting | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
Obtain retrograde access via the common femoral artery (CFA) using a percutaneous micropuncture (21-gauge needle) system under ultrasound guidance. The CFA should be accessed immediately proximal to the femoral bifurcation in an area with minimal disease. The right CFA is the most convenient site for right-handed operators. The left CFA and brachial and radial arteries are alternative access sites. Ultimately, the safest and simplest access site to the target lesion should be employed.
The micropuncture sheath is then exchanged for a 5-Fr introducer sheath over the 0.035-in access wire.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




