Carotid Endarterectomy
Parth B. Amin
Timothy F. Kresowik
The carotid bifurcation in the neck is a frequent site of atherosclerosis. Thromboembolic events originating from atherosclerotic plaque at this location are a common cause of ischemic stroke. Fortunately, the disease is most often limited to the region of the bifurcation and is surgically accessible. Randomized clinical trials have established the efficacy of carotid endarterectomy (surgical plaque removal) for stroke prevention in patients who have high-grade stenosis of the proximal internal carotid artery.
SCORE™, the Surgical Council on Resident Education, has classified this as an “ESSENTIAL COMMON” procedure.
Steps in Procedure
Identify mastoid process and sternal notch
Incision parallels anterior border of sternocleidomastoid and curves medially at the inferior aspect toward the sternal notch
Mobilize medial border of sternocleidomastoid
Preserve great auricular nerve if possible
Expose medial border of internal jugular vein
Identify and ligate the facial vein
Expose common carotid artery and dissect lateral border of the internal carotid artery
Protect vagus nerve and identify hypoglossal nerve; divide branch from occipital artery if needed
Administer systemic heparin
Clamp the internal carotid artery, common carotid artery, and external carotid artery
Place arteriotomy on middle portion of common carotid and extend toward carotid bifurcation
Transect internal carotid artery off of the common carotid
Eversion endarterectomy of internal carotid artery
Feather to good endpoint; transect plaque at appropriate endpoint if needed
Separate and evert plaque from orifice of external carotid artery
Anastomosis from internal carotid artery to carotid bifurcation
Flush debris before completing suture line by opening each clamp
Restore circulation to external carotid artery first
Close wound in two layers
HALLMARK ANATOMIC COMPLICATIONS
Embolic stroke
Injury to marginal mandibular nerve
Injury to hypoglossal nerve
Injury to spinal accessory nerve
Injury to vagus nerve
LIST OF STRUCTURES
Sternocleidomastoid muscle
Mandible
Mastoid process
Clavicular head
Langer’s lines
Platysma muscle
Parotid gland
Sternocleidomastoid muscle
Mastoid process
Clavicular head
Langer’s lines
Platysma muscle
Parotid gland
External jugular vein
Great auricular nerve
Marginal mandibular branch of facial nerve
Internal jugular vein
Facial vein
Digastric muscle
Hypoglossal nerve (XII)
Sternocleidomastoid branch of occipital artery
Ansa cervicalis
Vagus nerve
Glossopharyngeal nerve (IX)
Omohyoid muscle
Common carotid artery
Internal carotid artery
External carotid artery
Superior thyroid artery
Superior laryngeal nerve
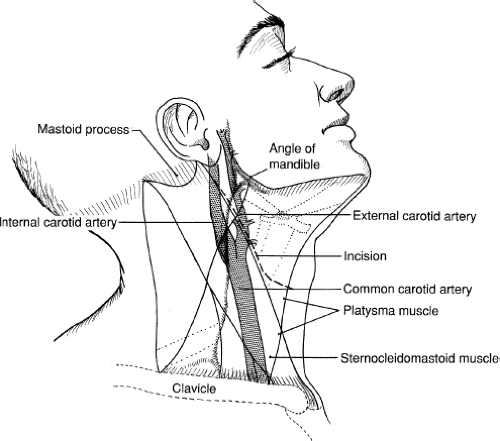
Regional Anatomy and Skin Incision (Fig. 9.1)
Technical Points
Preoperative determination of extent of disease and location of the carotid bifurcation, through either duplex ultrasound imaging or angiography, allows the skin incision to be planned for optimal access. The description that follows would apply to patients whose carotid bifurcation is in the typical position in the mid-neck and in whom the disease does not extend unusually far distally or proximally.
Position the patient with the neck extended and the head rotated to the side opposite the procedure. It is also helpful to have the head of the bed elevated about 30 degrees to decrease venous pressure and bleeding. The most important landmark for planning the incision is the anterior border of the sternocleidomastoid muscle, which can be visualized or palpated. Initiate the distal end of the incision along this border at the level of the angle of the mandible or 2 to 3 cm from the mastoid process. The upper portion of the incision should follow the border of the sternocleidomastoid muscle. At a point two-thirds of the distance between the mastoid process and the head of the clavicle, curve the incision into a more transverse direction to produce a better cosmetic result than the traditional straight incision.
Anatomic Points
The incision described previously allows the best balance between exposure and cosmesis. Langer’s lines in the neck are predominately horizontal, and making the inferior portion of the incision more transverse results in a better scar that follows the normal skin creases.
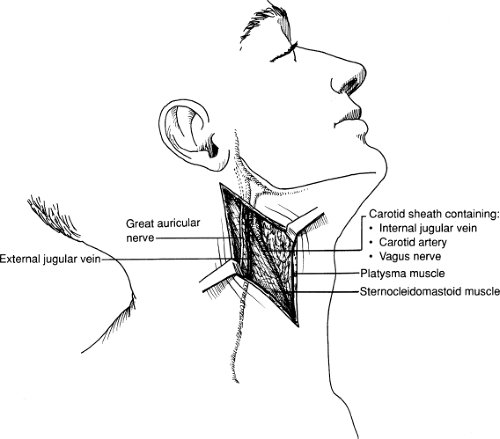
Exposure of the Sternocleidomastoid Muscle (Fig. 9.2)
Technical Points
Deepen the skin incision through the subcutaneous tissue and platysmal layer. Mobilize the medial border of the sternocleidomastoid muscle along the entire length of the incision. If the incision is extended superiorly, the tail of the parotid gland is encountered. If necessary for exposure, this portion of the parotid can be mobilized along the inferior and posterior aspects of the gland. The external jugular vein and great auricular nerve may be encountered at this level. The external jugular vein may be ligated. Preserve the great auricular nerve if possible. The dissection plane should remain over the medial border of the sternocleidomastoid muscle and not drift anteriorly toward the mandible because injury to the marginal mandibular branch of the facial nerve could result. Near the upper end of the incision, an arterial branch from the occipital artery going to the sternocleidomastoid muscle may be encountered and should be divided. This arterial branch usually loops over the hypoglossal nerve in its course from the occipital artery, and division allows the hypoglossal nerve to retract medially away from the dissection plane.
If more proximal exposure of the common carotid is necessary, develop a subplatysmal flap at the inferior end of the
incision to allow continued mobilization of the medial border of the sternocleidomastoid muscle to its clavicular insertion despite the transverse course of the skin incision.
incision to allow continued mobilization of the medial border of the sternocleidomastoid muscle to its clavicular insertion despite the transverse course of the skin incision.
Anatomic Points
The platysma muscle has little functional importance but is the division between a plane superficial to the muscle, which is devoid of significant neurovascular structures, and the plane deep to the muscle that contains nerves that should be preserved if possible. The great auricular nerve is a sensory branch of C2 and C3 that parallels the external jugular vein. Sacrifice or injury to the great auricular nerve leads to numbness or paresthesia of the ear. The marginal mandibular branch of the facial nerve normally parallels the ramus of the mandible but can extend as much as 2.5 cm inferior to the mandible. The nerve is a motor branch to the muscles of the corner of the mouth. Injury to this nerve can lead to a significant cosmetic and functional impairment, with ipsilateral drooping of the corner of the mouth and drooling. Keeping the dissection plane along or posterior to the border of the sternocleidomastoid muscle will usually avoid direct injury to this nerve. This nerve can also be injured by injudicious placement of mechanical retractors against the mandible.
Exposure of the Carotid Sheath and Internal Jugular Vein (Fig. 9.3)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree