Candidiasis
Irina Margaritescu, MD, DipRCPath
Bruce R. Smoller, MD
Key Facts
Terminology
Common superficial infection of skin and mucous membranes caused by yeasts of genus Candida
Etiology/Pathogenesis
C. albicans is the predominant causal organism of most candidal infections
Clinical Issues
Common in groups at risk, such as patients who are immunocompromised
Various mucosal and cutaneous manifestations of which oral thrush and candidal intertrigo are most common
Other forms include chronic mucocutaneous candidiasis, genital candidiasis, candidal paronychia and onychomycosis, congenital candidiasis, and disseminated candidiasis
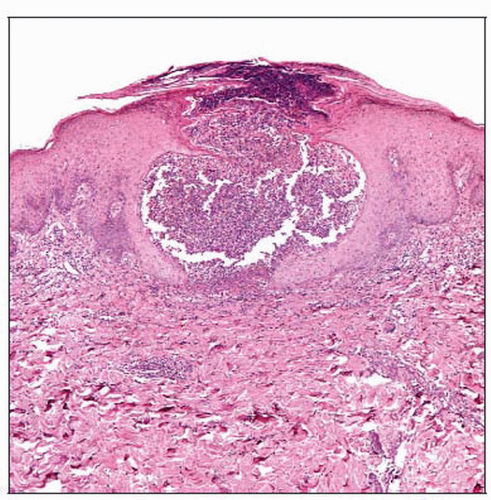
Microscopic Pathology
Neutrophils scattered in epidermis with formation of spongiform or subcorneal pustules
Orthokeratosis and parakeratosis
Pseudohyphae and spores
Blue streaks oriented perpendicular to skin surface
Mostly in zones of parakeratosis
Ancillary Tests
Fungal elements best visualized with periodic acid-Schiff stain
TERMINOLOGY
Synonyms
Candidiasis
Moniliasis
Thrush
Oidiomycosis
Definitions
Common superficial infection of skin and mucous membranes caused by yeasts of genus Candida
ETIOLOGY/PATHOGENESIS
Infectious Agents
C. albicans is the predominant causal organism of most candidal infections
Oval yeast 2-6 by 3-9 µm in size
Produce budding cells, pseudohyphae, and true hyphae
Other species, including C. krusei, C. glabrata, C. dubliniensis, and C. inconspicua isolated from severely immunocompromised patients
Pathogenesis
C. albicans is not a normal cutaneous saprophyte but usually colonizes oropharynx, gastrointestinal tract, and vagina
Alteration in host defenses, either localized or generalized, allows organism to become pathogenic
Factors predisposing to infection include
Mechanical factors (trauma, occlusion)
Nutritional factors (iron deficiency, malnutrition)
Physiologic alteration (menses, pregnancy)
Systemic illnesses (diabetes mellitus, malignancy, uremia, immunodeficiency states)
Iatrogenic causes (antibiotics, steroids)
Virulence factors include surface adhesion molecules and proteinase enzymes
CLINICAL ISSUES
Epidemiology
Incidence
Common in groups at risk (immunocompromised patients)
Age
Any age
Gender
Both sexes
Presentation
Various mucosal and cutaneous manifestations
Oral candidiasis may appear in acute or chronic forms
Acute pseudomembranous candidiasis or thrush
Most common form of oral candidiasis
Occurs in neonates or in adults usually secondary to local or general predisposing factors
Discrete white patches on buccal mucosa, tongue, palate, and gingivae, which, when removed, leave a raw and brightly erythematous surface
Acute erythematous (atrophic) candidiasis
May occur de novo or after sloughing of pseudomembrane
Commonly associated with antibiotics and steroid treatments
Marked soreness and depapillated erythematous areas on dorsal surface of tongue
Chronic pseudomembranous candidiasis
Occurs principally in immunocompromised patients
Very persistent lesions
Very similar clinically to acute pseudomembranous form
Chronic erythematous candidiasis (denture stomatitis)
Associated with loss of dentition, poorly fitting dentures, malocclusion, and vitamin deficiency
Erythema and edema of palatal mucosa that contacts dentures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree