Bronchoscopy
M. Victoria Gerken
Phillip C. Camp Jr.
Fiberoptic bronchoscopy is frequently performed for diagnosis and for management of secretions. This chapter describes how to access various segments of the bronchial tree with both the fiberoptic and the rigid bronchoscope. References at the end detail special additional procedures such as endobronchial ultrasound (used to stage lung cancer) and bronchoalveolar lavage for pneumonia.
SCORE™, the Surgical Council on Resident Education, has classified bronchoscopy as an “ESSENTIAL COMMON” procedure.
STEPS IN PROCEDURE
Flexible Fiberoptic Bronchoscopy
Provide adequate topical anesthesia and sedation, and ensure adequate monitoring
Introduce fiberoptic bronchoscope through anesthetized naris
Identify larynx and vocal cords
Pass scope through cord into proximal trachea
Look first where the lesion is suspected on the basis of imaging studies; obtain biopsies or brushings if desired
Then examine remainder of tracheobronchial tree in systematic fashion
Rigid bronchoscopy
General anesthesia, patient positioned with neck in slight hyperextension
Ventilation port is used by anesthesiologist to maintain ventilation during procedure
Introduce scope through mouth, elevate epiglottis and pass through cords
Continuously support the rigid bronchoscopy and avoid sudden movements
Advance scope along tracheobronchial tree to desired location
HALLMARK ANATOMIC COMPLICATIONS
Incomplete examination or inability to cannulate selected segmental bronchus
Bleeding from biopsy
LIST OF STRUCTURES
Inferior nasal meatus
Nasopharynx
Oropharynx
Pharynx
Laryngeal aditus
Larynx
Vocal cords
Cricoid cartilage
Aryepiglottic folds
Trachea
Carina
Right Main Stem Bronchus
Bronchus intermedius (intermediate bronchus)
Left Main Stem Bronchus
Right Lung
Right upper lobe
Right middle lobe
Right lower lobe
Left Lung
Left upper lobe
Lingula
Left lower lobe
Bronchopulmonary segments
Left and right vagus nerves
Stomach
Cardioesophageal junction
Spleen
Gastrosplenic (lienogastric) ligament
Fiberoptic Bronchoscopy
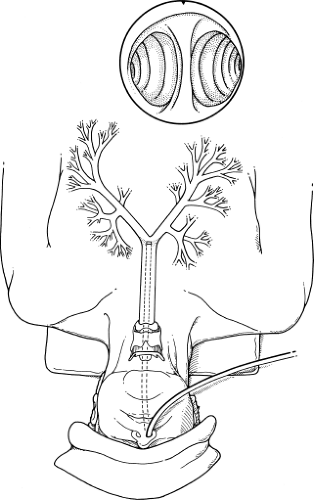
Introduction of the Bronchoscope (Fig. 25.1)
Technical Points
Anesthesia is crucial for successful fiberoptic bronchoscopy. There are certain situations in which it is expedient to perform this procedure under general anesthesia (i.e., when the patient cannot tolerate topical anesthesia, when the patient is anesthetized for another reason, or before a thoracotomy that is being performed to resect a small, peripheral nodule). Although general anesthesia does allow the endoscopist to examine the periphery closely without having to deal with coughing, the proximal trachea and the cords cannot be examined in an intubated patient. This is especially pertinent when one is evaluating central lung lesions and when there is a possibility of involvement of the recurrent laryngeal nerve. However, more than half of the life-threatening complications stemming from bronchoscopy are related to hypoxemia, hypercapnia, respiratory depression (oversedation), and medication side effects. Each clinical scenario should be carefully considered.
Most diagnostic bronchoscopy procedures are performed using topical anesthesia. However, all too often, the inexperienced endoscopist fails to achieve adequate anesthesia and ends up with an incomplete bronchoscopy because the patient is coughing and is clearly dyspneic. With an adequate balance of sedation (i.e., with diazepam or midazolam hydrochloride), adequate analgesia and antitussive management (meperidine, morphine), and adequate topical anesthesia of the naris, the posterior pharynx, the aryepiglottic folds, and the cords, the average patient will be able to tolerate the procedure with little or no coughing, dyspnea, or agitation.
Place viscous lidocaine jelly on a series of cotton-tipped applicators and use these to anesthetize the naris, progressing slowly to the back of the nasopharynx as an anesthetic effect is achieved. Anesthetize the rest of the airway by connecting an atomizer filled with 4% lidocaine to a high-flow oxygen system with a Y connector. The anesthetic can then be sprayed gently over the mucous membranes with good control.
The use of intravenous sedation, careful monitoring of pulse oximetry, adequate topical anesthesia, and antisialogogues (atropine, glycopyrrolate) when indicated will allow careful and systematic examination of the proximal tracheobronchial tree. With the fiberoptic bronchoscope, you should be able to reach, without difficulty, the orifices of the third order of bronchi in all lobes.
Introduce the fiberoptic bronchoscope through the anesthetized naris. Pass the instrument into the back of the oropharynx and identify the larynx and vocal cords. Ask the awake patient to speak to confirm equal and full movement of the true cords. You may wish to inject additional topical anesthetic at this point to ensure its direct application to the cords. Under direct visualization, pass the fiberoptic bronchoscope through the cords into the proximal trachea. Inspect the area for neoplasms (both tumors and granulomas), excessive collapse of the trachea (tracheomalacia), points of external compression, and injuries (erosions, trauma, hematoma, disruption). The U shape of the tracheal cartilages and the comparatively flat, softer, membranous posterior wall make easy landmarks for maintaining proper orientation. The carina should appear to have a very acute angle with a sharp edge. Blunting of this angle can be seen with disease involving the subcarinal lymph nodes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree