Breast Biopsy, Lumpectomy, and Partial Mastectomy
This chapter describes how palpable and nonpalpable masses are excised. Every effort should be made before surgery to determine whether the mass is benign or malignant, because this determines the width of margins necessary. With the wealth of image-guided percutaneous biopsy techniques available, as well as fine needle aspiration for cytology, it is rarely necessary to excise a mass simply to get a diagnosis.
When the lesion is not palpable, or when resection is needed after core biopsy, the lesion must be localized by hookwire placement under radiographic or ultrasound guidance (see Fig. 16.3). Ultrasound-guided localization is an alternative described in Chapter 15.
The chapter also describes how lumpectomy and partial mastectomy are performed for the treatment of breast cancer or ductal carcinoma in situ (DCIS).
SCORE™, the Surgical Council on Resident Education, classified breast biopsy with or without needle localization, and partial mastectomy, as “ESSENTIAL COMMON” procedures.
STEPS IN PROCEDURE
Palpable Mass
Circumareolar incision where feasible
Incision directly over mass if necessary
Raise flaps
Transfix mass with traction suture
Excise with appropriate margin, orient specimen
Nonpalpable Mass with Needle/Localization
Inspect localization radiographs and trajectory of needle, estimate position of lesion
Make incision over likely location of mass
Circumareolar incision may be used for lesion close to areolar margin
Deliver wire into wound
Transfix tissue around wire with traction suture
Excise tissue around wire, leaving tip of wire to final part of dissection
Orient specimen
Radiograph specimen to determine adequacy of excision
Larger margin and more careful excision of all abnormal tissue needed for DCIS or breast cancer (partial mastectomy)
Obtain hemostasis
Close incision in layers without a drain
HALLMARK ANATOMIC COMPLICATIONS
Missed lesion or failure of localization (needle localized)
Broken wire, necessitating retrieval with metal detector
Hematoma
LIST OF STRUCTURES
Breast
Nipple areola
Axillary tail of Spence
Choice of Incision (Fig. 16.1)
Technical Points
For most easily palpable lesions that lie within several centimeters of the areola, a circumareolar incision is appropriate for obtaining a biopsy specimen. However, biopsy of ill-defined masses that are not easily reached using this approach should be accomplished through an incision placed directly over the mass. In such cases, the incision should be gently curved in the upper or lower parts of the breast, and should be transverse, or nearly so, in the medial or lateral aspects. This allows the scar to be hidden by clothing or readily incorporated into a mastectomy incision should that procedure be indicated.
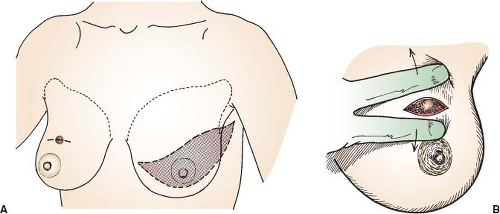 Figure 16.1 Choice of incision. A: Incision made as low as possible in natural skin crease. B: Incision in skin crease directly over palpable mass. |
Radial incisions, once advocated because they parallel the underlying duct structure of the breast, yield poor cosmetic results and should be used only for very medial or lateral lesions. When planning the incision, remember that the biopsy site will have to be excised with a skin margin should subsequent mastectomy be required. For this reason, inframammary incisions, although cosmetically appealing, are generally avoided.
Choose a site for incision and infiltrate the area with local anesthetic. If the mass becomes difficult to palpate after the skin preparation has been done, wash the skin of the breast with sterile saline and palpate by sliding gloved fingers over the wet skin.
Anatomic Points
The breast, which is wholly contained within superficial fascia, extends from the second rib superiorly to the sixth rib inferiorly and from the sternum to the midaxillary line. The axillary tail of Spence is an extension of breast tissue into the axilla. The breast is composed of 15 to 20 glandular lobes and adipose tissue arranged radially around the nipple-areolar complex. These are separated by fibrous septa, fibers of which attach to the deep surface of the skin and to the deep layer of the superficial fascia (suspensory ligaments of Spence). The glandular tissue of the lobes, each based on a lactiferous duct that drains at the apex of the nipple, tends to be located more centrally, whereas the adipose tissue tends to be located more peripherally.
A circumareolar incision produces a scar that is almost hidden in the abrupt change in skin pigmentation at the areolar margin. If the location of the lesion makes this impossible, the incision should approximate the direction of the skin cleavage lines. These lines are concentrically arranged around the nipple, although in pendulous breasts, the effects of gravity are superimposed on this pattern. The surgeon should be aware of the underlying radial breast architecture and should restrict the initial incision to the skin.
Biopsy of a Palpable Mass (Fig. 16.2)
Technical Points
Make a circumareolar incision and raise a flap (generally, 0.5 cm in thickness) in the cleavage plane between the subcutaneous tissue and the breast. This is the same plane in which mastectomies are performed. Place retractors to pull the incision closer to the mass. Identify the mass by palpation. If necessary, cut through the overlying breast tissue to expose the mass. Place a traction suture of 2-0 silk in a figure-of-eight fashion through the mass. (Use a curved cutting needle because the tough, fibrous breast tissue will bend a tapered-point needle.) Pull up on the traction suture to elevate the mass into the field. Excise the mass by sharp dissection using a knife or Mayo scissors. Avoid overzealous use of electrocautery on the biopsy specimen because this can render assessment of margins difficult, particularly in borderline lesions. Take care not to violate the pectoral fascia by cutting too deeply because this fascia provides a natural barrier that will help to prevent contamination of the mastectomy field with spilled tumor cells if subsequent mastectomy is performed.
Feel both the excised mass and the residual breast cavity to ascertain that the palpable lesion has been removed. Request that receptor and tumor markers be done if the biopsy is positive for carcinoma. Some laboratories may require that fresh tissue be submitted; know the requirements of your pathologist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


