Branchial Cleft Cyst
Lester D. R. Thompson, MD
Key Facts
Terminology
Branchial cleft cyst refers to congenital developmental lateral cervical cyst derived from remnants of 2nd branchial apparatus
Etiology/Pathogenesis
Failure of obliteration of cervical sinus results in 2nd branchial cleft remnant (cyst, sinus, or fistula)
Clinical Issues
Comprises ˜ 20% of all congenital cervical cysts
Bimodal presentation (< 5 years; 20-40 years)
Waxing and waning, painless, compressible, cervical swelling
Enlarges after upper respiratory tract infection
Along anterior border of sternocleidomastoid muscle
Initial work-up of suspected branchial cleft anomaly (in order)
Intravenous or oral antibiotics (if infected), FNA, endoscopy &/or radiographic studies, surgery
Complete surgical excision yields a low recurrence risk
Microscopic Pathology
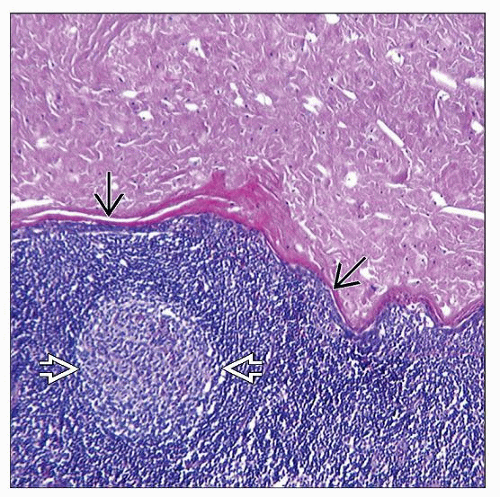
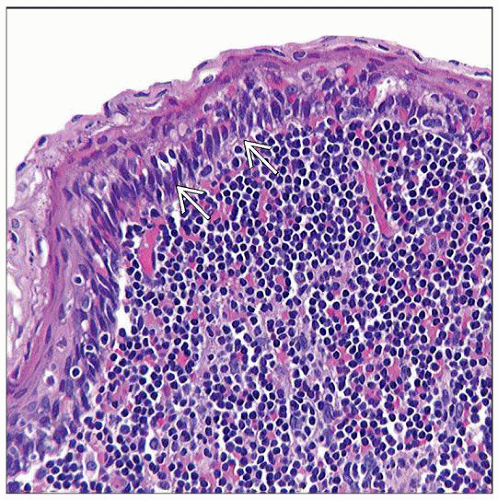
Usually a unilocular cyst
Cyst lined by various types of epithelium (90% stratified squamous)
Lymphoid aggregates in cyst wall
Top Differential Diagnoses
Epidermal inclusion cyst, metastatic cystic squamous cell carcinoma, bronchogenic cyst, metastatic thyroid papillary carcinoma, cervical thymic cyst
TERMINOLOGY
Abbreviations
Branchial cleft cyst (BrCC)
Definitions
By convention, “branchial cleft cyst” refers to congenital developmental lateral cervical cyst derived from remnants of 2nd branchial apparatus
Encompasses branchial cyst, sinus, or fistula
ETIOLOGY/PATHOGENESIS
Branchial Apparatus
Precursor of many head and neck structures
2nd branchial arch overgrows 2nd, 3rd, and 4th clefts
This overgrowth forms “cervical sinus”
Embryogenesis is usually complete by 6-7 weeks of gestation
Failure of obliteration of cervical sinus results in 2nd branchial cleft remnant (cyst, sinus, or fistula)
2nd branchial cleft fistula extends from skin anterior to sternocleidomastoid muscle (SCM), through carotid artery bifurcation to terminate in tonsillar fossa
3rd and 4th branchial cleft cysts are very uncommon (< 5%)
Recurrent neck abscess or acute suppurative thyroiditis
Vast majority on left side (90-95%)
Some posit cystic transformation of cervical lymph nodes
Especially in adults
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon
Still, BrCC is one of the most commonly encountered congenital anomalies in pediatric otolaryngic practice
Thyroglossal duct cysts are most common
BrCC accounts for ˜ 20% of all congenital cervical cysts
Cysts > > sinuses (3:1)
About 80-90% of all branchial cleft anomalies are 2nd branchial cleft cysts
Age
Bimodal presentation
< 5 years old (25%)
20-40 years old (75%)
˜ 1% in patients > 50 years old
Gender
Equal sex distribution
Site
Lateral neck near mandibular angle
Along anterior border of SCM
Anywhere from hyoid bone to suprasternal notch
Curiously, left-sided predominance for 4th branchial anomalies (> 90%)
Presentation
Painless cervical swelling
Along anterior border of SCM
Often present for long duration
May be painful (if infected)
Waxing and waning lesion
Frequently enlarges in concert with upper respiratory tract infection
Patients present during phase of recent enlargement
May lie dormant (clinically silent) for years
Compressible, fluctuant
Mucoid or pus-like secretions from sinus tract skin opening (when opening is present)
Clinically, some lesions may mimic parotid mass or odontogenic infection
Bilateral lesions are usually identified in syndromic or familial association
Clinically, 1st or 4th BrCC more likely to have incision and drainage procedures, resulting in “recurrence”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree