Below-knee Amputation
Most amputations are performed for ischemia. The choice of the level of amputation requires mature judgment. Although it is important to salvage as much length as possible, a poor initial choice of level may doom the patient to a second amputation, often at a significantly higher level. References at the end discuss factors to consider in selecting an amputation site as well as the utility of several commonly performed tests.
When below-knee amputation is performed for ischemia, the stump should be made long enough to allow fitting of a prosthesis, but not so long that viability is sacrificed. Below-knee amputation that is performed for trauma, in the presence of normal arteries, may be performed at a lower level.
In this chapter, the standard procedure for below-knee amputation, as performed for ischemia, is described. References at the end of the chapter detail alternative techniques, including amputation for trauma or tumor.
Steps in Procedure
Skin incision should provide longer posterior flap than anterior flap
Incise anteriorly and laterally, but not posteriorly at this stage, to limit blood loss
Preserve as much length as possible
Ligate and divide greater saphenous vein
Divide all soft tissues to tibia anteriorly and through fascia of muscles laterally
Strip periosteum from tibia circumferentially
Divide tibia 1 to 2 cm above level of skin incision
Divide fibula several centimeters higher than tibia
Smooth ends of bone
Suture-ligate and divide posterior tibial artery and vein
Divide common peroneal nerve cleanly and allow to retract
Develop posterior flap
Complete posterior skin incision
Ligate and divide lesser saphenous vein
Obtain hemostasis and tailor skin flaps
Close in layers
Hallmark Anatomic Complications
Ischemia of stump
Neuroma formation
List of Structures
Tibia
Tibial tuberosity
Fibula
Greater saphenous vein
Lesser saphenous vein
Saphenous nerve
Common peroneal nerve
Superficial fascia
Deep fascia
Interosseous membrane
Gastrocnemius muscle
Soleus muscle
Tibialis anterior muscle
Extensor digitorum longus muscle
Extensor hallucis longus muscle
Peroneus longus muscle
Tibialis posterior muscle
Tendon of plantaris muscle
Popliteal Artery and Vein
Anterior tibial artery and vein
Posterior tibial artery and vein
Peroneal artery and vein
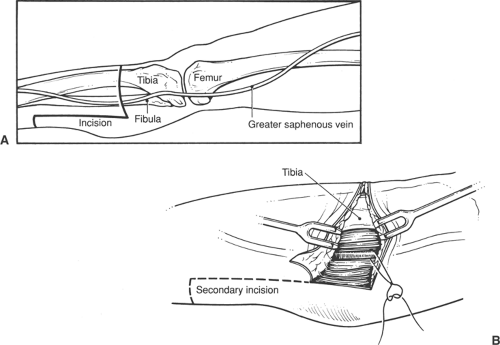
Skin Incision and Development of Flaps (Fig. 104.1)
Technical Points
Plan a skin incision with a long posterior flap. The length of the posterior flap should approximate the transverse diameter of the leg. As extra length of flap can always be trimmed; it is advisable to make the flap too long at the initial incision. Divide the minimal soft tissues anterior to the tibia. Plan to divide the tibia about four fingerbreadths below the tibial tuberosity. If the amputation is being performed for trauma, a longer stump may be tailored. Generally, when amputation is done for ischemia, a shorter stump is desirable.
Identify and ligate the greater saphenous vein in the medial aspect of the anterior incision. Divide all soft tissues down to the tibia anteriorly and through the fascia of the muscles laterally.
To limit blood loss, do not create the posterior skin incision at this point.
Anatomic Points
The division of the tibia about four fingerbreadths inferior to the tibial tuberosity corresponds to approximately the level of the greatest circumference of the leg. At this location, the greater saphenous vein and accompanying saphenous nerve are located in the superficial fascia just posterior to the medial border of the tibia—that is, in the fascia overlying the tibial origin of the soleus muscle. No important structures lie in the superficial fascia anterior to the greater saphenous vein. The anteromedial surface of the tibia lies just deep to the superficial fascia. Hence, the anterior border of the tibia is a useful landmark, and no muscles must be divided to expose it.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree