Axillary Node Dissection
Laura A. Adam
Neal Wilkinson
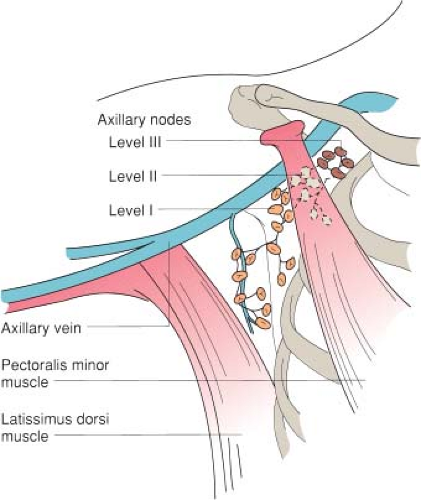
Axillary lymph node dissection typically refers to the more limited resection of topographic group I and group II axillary lymph nodes (Fig. 21.1). It is most commonly performed for breast cancer, but can be used for treatment of other malignancies like melanoma. When performed in conjunction with mastectomy it is termed as modified radical mastectomy (see Chapter 18), but it is often performed as an isolated axillary node dissection with lumpectomy. Often a sentinel lymph node biopsy will have been performed prior to axillary lymph node dissection, either as a separate surgical procedure or during the initial phase of the same operation.
This chapter first discusses the technical modifications required when axillary node dissection is done alone followed by description of a more limited axillary node sampling procedure previously used in staging of breast carcinomas. This procedure is now rarely performed following the widespread use of sentinel lymph node biopsy.
SCORE™, the Surgical Council on Resident Education, did not specifically classify Axillary node dissection.
STEPS IN PROCEDURE
Position patient supine, with arm extended on arm board
Transverse incision below hair-bearing area or oblique incision just behind lateral edge of pectoralis major muscle
Raise flaps
Identify lateral edge of pectoralis major muscle
Dissect under pectoralis major muscle, preserving median pectoral neurovascular bundle
Identify pectoralis minor muscle and dissect under it (sometimes, it may be divided or excised to facilitate dissection)
Identify axillary vein and trace it laterally
Identify long thoracic nerve and incise fascia lateral to it; mobilize the nerve medially
Identify thoracodorsal neurovascular bundle and preserve it
Sweep all fatty node-bearing tissue inferiorly and laterally, preserving nerves and axillary vein
Orient specimen
Obtain hemostasis and place closed suction drains
Close incision in layers
Axillary Sampling
Shorter but similar incision
Dissection is limited to level I and some level II nodes
Preserve nerves as noted above
HALLMARK ANATOMIC COMPLICATIONS
Injury to median pectoral nerve
Injury to long thoracic nerve (winged scapula)
Injury to thoracodorsal nerve
Injury to axillary vein
Division or injury to intercostobrachial nerve
LIST OF STRUCTURES
Pectoralis major muscle
Pectoralis minor muscle
Clavipectoral fascia
Lateral pectoral nerve
Medial pectoral nerve
Thoracodorsal nerve
Long thoracic nerve
Axillary artery
Axillary vein
Thoracoacromial artery
Thoracodorsal vein
Axillary Node Dissection
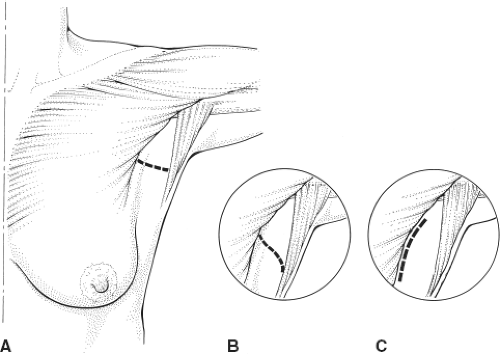
Choice of Incision and Elevation of Flaps (Fig. 21.2)
Technical Points
Position the patient with the arm extended on an arm board with a bump under the shoulder (see Chapter 18). If sentinel node biopsy has been performed at an earlier time, plan an incision that excises and extends the previous scar. It will, in general, be easiest to stay wide of the sentinel lymph node dissection field and dissect in fresh tissue around that field. Excising the old scar may help avoid going back into a scarred area. If sentinel node biopsy was done during the same operative procedure and returned positive, then simply extend the sentinel node incision in both directions. Again, allowing subsequent dissection to progress through fresh undissected planes is generally the safest strategy.
An oblique incision just lateral to the pectoralis major muscle provides excellent access to the axilla, and this lateral location allows the scar to fall behind the muscle, where it is less noticeable. A more cosmetically appealing transverse or U-shaped incision may also be used. A transverse incision should be planned to lie below the hair-bearing portion of the axilla. Patient habitus and location of sentinel lymph node often determine incision preference. As with sentinel node biopsy, in corpulent patients an incision in the line between the axillary fat pat and the breast fat may provide the easiest access to the axilla (see Chapter 20).
After incising the skin, create skin flaps to expose the subcutaneous tissues.
Anatomic Points
Discrete superficial and deep fascia is not encountered in the axilla. Instead, the axillary fascia (derived from the fascia of the pectoralis major, latissimus dorsi, serratus anterior muscles, and investing the muscles of the arm) is adherent to the superficial fascia and is, in the hollow of the armpit, along with the suspensory ligament of the axilla, a continuation of the clavipectoral fascia.
The axillary lymph nodes are predominantly located on the medial side of the axillary neurovascular bundle, and along the medial axillary wall. Terminology is complicated by multiple nomenclature systems including the anatomic system, Haagensen’s system (explained later in this chapter), and the surgeon’s topographic levels I to III (as shown in Fig. 21.1). The anatomic lateral group on the third part of the axillary neurovascular bundle drains the upper limb. The subscapular group located around the subscapular artery and vein drains the shoulder and posterior thorax. The pectoral group associated with the lateral thoracic vessels along the inferolateral border of the pectoralis major muscle drains the anterior thoracic wall including the lateral breast. These three groups drain into the central group lymph nodes located on the second part of the axillary neurovascular bundle which then further joins with the upper outer quadrant of the breast to drain into the apical group.
Surgeons commonly use a different terminology (topographic) for axillary lymph nodes. Topographic group I nodes include the pectoral, subscapular, and lateral nodes. These are the nodes lateral to the pectoralis minor muscle. Topographic group II nodes are under the pectoralis minor muscle and correspond to the central nodes, whereas topographic group III nodes are medial to the pectoralis minor muscle and correspond to the apical nodes (see Fig. 21.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree