Autoimmune Pancreatitis
Mari Mino-Kenudson, MD
Key Facts
Terminology
Fibroinflammatory disease of presumed autoimmune etiology that affects pancreas
Often elevated serum IgG4
Similar fibroinflammatory process often affects other organs such as bile ducts, salivary glands, retroperitoneum, and lymph nodes
Associated with many other autoimmune diseases
Image Findings
Diffusely enlarged gland
Delayed (rim) enhancement
Attenuated, irregular main pancreatic duct
Macroscopic Features
Enlarged, firm pancreas
Variably present mass lesion
May mimic adenocarcinoma
Microscopic Pathology
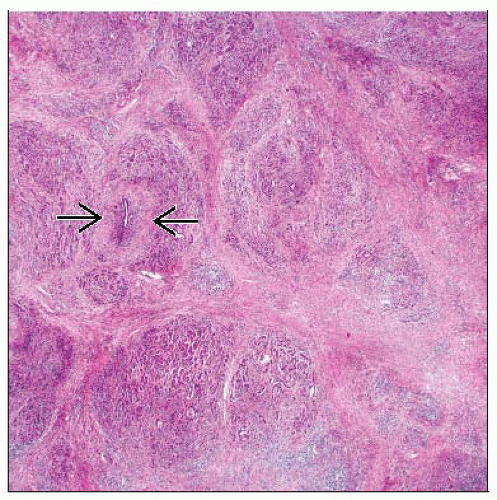
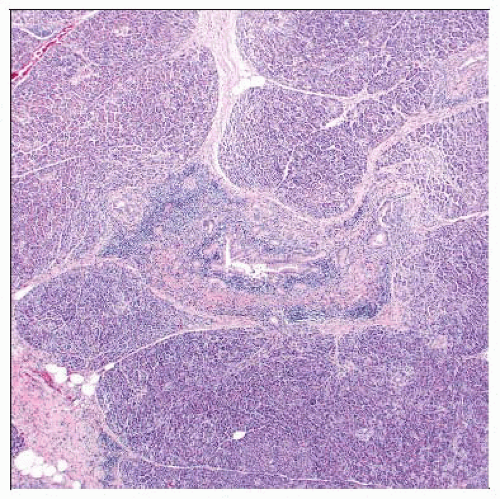
Dense lymphoplasmacytic infiltration centered around main and interlobular pancreatic ducts
Periductal, lobular, and perilobular fibrosis
Obliterative phlebitis and venulitis
Granulocytic epithelial lesions
IgG4(+) plasma cells
Top Differential Diagnoses
Pancreatic cancer
Other forms of chronic pancreatitis
TERMINOLOGY
Abbreviations
Autoimmune pancreatitis (AIP)
Synonyms
Lymphoplasmacytic sclerosing pancreatitis (LPSP)
Idiopathic duct-centric chronic pancreatitis (IDCP)
Primary sclerosing pancreatitis
Nonalcoholic duct destructive chronic pancreatitis
Definitions
Fibroinflammatory disease of presumed autoimmune etiology that affects pancreas
Similar fibroinflammatory process often affects other organs such as bile ducts, salivary glands, retroperitoneum, and lymph nodes
Associated with many other autoimmune diseases
Specific antigenic trigger unknown
CLINICAL ISSUES
Presentation
Jaundice
Weight loss
Vague abdominal pain
Laboratory Tests
Elevated serum IgG4
Elevated pancreatic enzymes
ANA often positive
Treatment
Surgical approaches
Surgically resected when differentiation from pancreatic cancer is difficult or impossible
Drugs
Steroids
Prognosis
Steroid therapy is usually very effective
Natural regression seen in some cases
Recurrence reported in 6-26%
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree