Appendectomy and Resection of Meckel Diverticulum
The anatomy of the lateral abdominal wall, including the rectus sheath and the right lower quadrant, is described in this chapter. The laparoscopic approach to the appendix and Meckel diverticulum is given in Chapter 95.
SCORE™, the Surgical Council on Resident Education, classified open appendectomy as an “ESSENTIAL COMMON” procedure.
STEPS IN PROCEDURE
Make small, obliquely oriented incision over McBurney point or over mass (if palpable)
Divide each layer by splitting or incising parallel to fibers
Deliver appendix into wound and confirm diagnosis
Serially clamp and tie appendiceal mesentery
Crush base of appendix with clamp and ligate with 0 chromic
Amputate appendix
Invert stump with purse string or Z stitch
Suction and irrigate field
Close incision in layers
If Appendix Appears Normal:
Remove appendix
Run small bowel for at least 1.2 m (4 feet)
Check pelvic organs (female), colon
Further exploration is determined by character of peritoneal fluid
HALLMARK ANATOMIC COMPLICATIONS
Missed pathology due to small incision when appendix normal
LIST OF STRUCTURES
Anterosuperior iliac spine
Umbilicus
McBurney point
Camper fascia
Scarpa fascia
External oblique muscle and aponeurosis
Rectus abdominis muscle
Rectus sheath
Semilunar line
Arcuate line (of Douglas)
Transversus abdominis muscle
Transversalis fascia
Iliohypogastric nerve
Subcostal nerves
Cecum
Appendix
Mesoappendix
Appendicular artery
Ileocolic artery
Ileocecal fold
Meckel diverticulum
Skin Incision (Fig. 94.1)
Technical Points
Always gently palpate the abdomen after the patient is intubated under anesthesia. You may be able to feel a mass that was inapparent while the patient was conscious and guarding. If a mass is palpable in the right lower quadrant after induction of anesthesia, make the incision over the mass.
More commonly, no mass is felt, and the skin incision is then centered by two fixed anatomic landmarks: The anterosuperior iliac spine and the umbilicus. Draw a line from the umbilicus to the anterosuperior iliac spine. McBurney point lies one-third of the distance from the anterosuperior iliac spine. The classic McBurney incision is made perpendicular to this line. The incision may be modified to follow the local lines of skin tension, as indicated, but it should pass through McBurney point. A Rockey-Davis incision is made over McBurney point, but is directed in a nearly transverse direction. This incision yields a good cosmetic result because it parallels Langer’s lines. It also more nearly approximates the direction of the major cutaneous nerves of the region, and it is easy to extend this incision should unexpected pathology be encountered at laparotomy.
Anatomic Points
The anterosuperior iliac spine presents as a prominence in slender individuals, but may take the form of a depression in obese patients. It is a constant, palpable landmark. The lateral border of the rectus abdominis muscle may be visible as the semilunar line. This begins inferiorly at the pubic tubercle and curves laterally as it ascends. At the level of the umbilicus, the semilunar line is about 7 cm from the midline and lies about halfway between the midline and the side of the body.
Generally, in this region, one will be able to identify a distinct division of the superficial fascia into two layers: The more superficial layer of fatty areolar tissue, which is Camper fascia, and the deeper, membranous layer, which is Scarpa fascia.
Muscle-Splitting Incision (Fig. 94.2)
Technical Points
The external oblique muscle and its aponeurosis form the first layer of the abdominal wall (which is encountered as the incision is deepened). Open each layer of the abdominal wall by splitting, rather than cutting, the muscular and aponeurotic fibers. The resulting muscle-splitting incision is called a gridiron
incision. Because each layer is opened parallel to the muscle fibers and hence in the direction of maximum tension when the fibers contract, the resulting incision is very strong, and hernias are rare.
incision. Because each layer is opened parallel to the muscle fibers and hence in the direction of maximum tension when the fibers contract, the resulting incision is very strong, and hernias are rare.
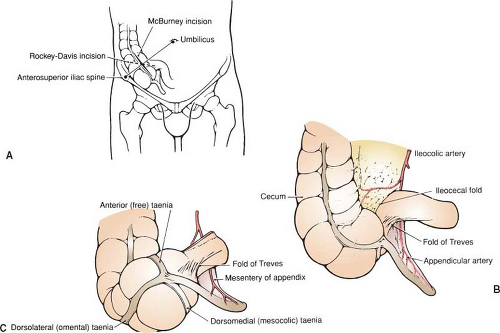 Figure 94.1 Skin incision. A: Typical location of McBurney and Rockey-Davis incisions. B: Regional anatomy. C: Relationship of appendix to taeniae of cecum. |
Medially, the external oblique aponeurosis contributes to the anterior rectus sheath. Usually, the rectus sheath forms the medial boundary of the fascial incision. If necessary, the rectus sheath may be incised. The rectus muscle can then be retracted medially to achieve additional exposure.
Anatomic Points
The fibers of the external oblique muscle run obliquely from above downward, and from lateral to medial (i.e., in the same direction as you would put your hands into your pockets). Fibers of the external oblique muscle terminate in its aponeurosis following a curved line from the semilunar line to approximately the anterosuperior iliac spine.
The major cutaneous nerves of the region are branches of the iliohypogastric and subcostal nerves.
Deepening the Incision (Fig. 94.3)
Technical Points
Split the fibers of the internal oblique and transversus abdominis muscles in turn by a combination of sharp and blunt dissection. Incise the fascia with a scalpel, cutting carefully, parallel to the fibers. Extend the cut by inserting partially closed Metzenbaum scissors and pushing, or by splitting bluntly with two fingers or a pair of hemostats. Medially, the sheath of the rectus abdominis muscle limits the extent of the split.
Anatomic Points
Note that the fibers of the internal oblique muscle are almost transverse at the level of this incision and that muscle extends much more medially than the muscular portion of the external oblique muscle. The aponeurosis of the internal oblique muscle contributes to the anterior rectus sheath along the entire length of this muscle and, by splitting, to the posterior rectus sheath above the arcuate line of Douglas.
Observe that fibers of the transversus abdominis muscle, in the operative field, almost parallel those of the internal oblique muscle. Muscle fibers proper terminate slightly more laterally than do those of the internal oblique muscle. The aponeurosis of the transversus abdominis muscle contributes fibers to the
anterior rectus sheath below the line of Douglas as well as to the posterior rectus sheath above.
anterior rectus sheath below the line of Douglas as well as to the posterior rectus sheath above.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



