Acid-Base and Electrolyte Disorders
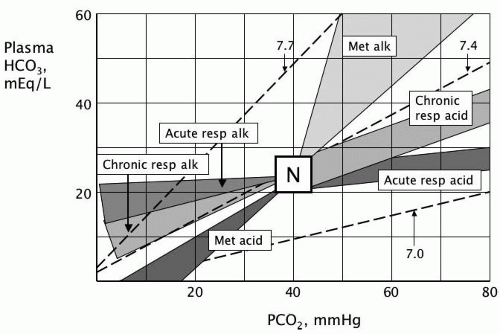
1-A. Acid-Base Nomogram
1-B. Metabolic Acidosis
Increased Anion Gap
Renal failure, acute or chronic
Ketoacidosis
Diabetic
Alcoholic
Starvation
Lactic acidosis (see 1-E)
Toxins
Aspirin
Methanol
Ethylene glycol
Toluene
Massive rhabdomyolysis
Inborn errors of metabolism (e.g., maple syrup urine disease, methylmalonic aciduria)
Normal Anion Gap
Gastrointestinal loss
Diarrhea
Ileal loop, ureterosigmoidostomy
Small bowel or pancreatic fistula or drainage
Ion-exchange resins (e.g., cholestyramine)
Calcium or magnesium chloride ingestion
Renal loss
Renal tubular acidosis (see 5-F)
Hypoaldosteronism
Potassium-sparing diuretics
Carbonic anhydrase inhibitors
Recovery phase of ketoacidosis
Rapid expansion of extracellular fluid volume with bicarbonate-free fluid (e.g., dilutional acidosis)
References
1. Shapiro JI, Kaehny WD. Pathogenesis and management of metabolic acidosis and alkalosis, p. 115. See Bibliography, 1.
2. Rose BD, p. 578. See Bibliography, 2.
1-C. Respiratory Acidosis
Neuromuscular Causes
Ingestion or overdose (e.g., tranquilizers, sedatives, anesthetics, anticholinesterases)
Cerebral, brainstem, or high spinal cord injury or infarct
Primary neuromuscular disease
Guillain-Barré syndrome
Myasthenia gravis
Amyotrophic lateral sclerosis
Poliomyelitis
Botulism
Tetanus
Myopathy involving respiratory muscles, especially:
Muscular dystrophy
Hypokalemic myopathy
Familial periodic paralysis
Primary hypoventilation
Sleep apnea syndrome
Diaphragmatic paralysis
Airway Obstruction
Upper airway
Laryngeal edema or spasm
Tracheal edema, stenosis
Obstructive sleep apnea
Lower airway
Mechanical
Foreign body
Aspirated fluid (e.g., vomitus)
Neoplasm
Bronchospasm
Acute
Chronic (e.g., chronic obstructive pulmonary disease)
Cardiopulmonary-Thoracic Causes
Cardiac arrest
Severe pneumonia
Severe pulmonary edema
Respiratory distress syndrome (infant or adult)
Restrictive lung disease (e.g., interstitial fibrosis)
Massive pulmonary embolism
Pneumothorax, hemothorax
Chest trauma
Kyphoscoliosis
Smoke inhalation
Inadequate mechanical ventilation
References
1. Rose BD, p. 647. See Bibliography, 2.
2. Kaehny WD. Pathogenesis and management of respiratory and mixed acid-base disorders, p. 154. See Bibliography, 1.
1-D. Anion Gap
Increased
Without acidosis
Administration of sodium salts of organic compounds (e.g., citrate, lactate, acetate)
High-dose penicillin or carbenicillin
Respiratory or metabolic alkalosis
Dehydration
With acidosis
Renal failure, acute or chronic
Ketoacidosis
Diabetic
Starvation
Alcoholic
Lactic acidosis (see 1-E)
Toxins
Aspirin
Methanol
Ethylene glycol
Toluene
Inborn errors of metabolism (e.g., maple syrup urine disease, methylmalonic aciduria)
Decreased
Hypoalbuminemia
Hypernatremia, severe
Dilution of extracellular fluid
Multiple myeloma
Hyperviscosity
Bromide ingestion
Hypercalcemia, hypermagnesemia (severe)
Lithium toxicity
References
1. Rose BD, p. 578. See Bibliography, 2.
2. Emmett M, Narins RG. Clinical use of the anion gap. Medicine. 1977;56:38.
1-E. Lactic Acidosis
Associated with Impaired Tissue Oxygenation
Shock (e.g., hypovolemic, cardiogenic, septic)
Hypoxemia, respiratory failure
Anemia, severe
Occurring in Absence of Apparent Hypoxemia or Circulatory Insufficiency
Diabetes, uncontrolled
Hepatic failure
Renal failure
Malignancy, especially leukemia or lymphoma
Drugs, toxins
Metformin
Methanol
Salicylates
Human immunodeficiency virus (HIV) nucleoside reversetranscriptase inhibitors (e.g., stavudine, zidovudine)
Iron
Strychnine
Ethanol
Cyanide
Carbon monoxide
Seizures
Excessive muscular activity (e.g., excessive exercise)
Alkalosis, respiratory or metabolic
D-Lactic acidosis (secondary to intestinal bacterial overgrowth)
Congenital enzyme deficiency (e.g., glycogen storage disease)
References
1. Shapiro JI, Kaehny WD. Pathogenesis and management of metabolic acidosis and alkalosis, p. 115. See Bibliography, 1.
2. Rose BD, p. 578. See Bibliography, 2.
3. Kreisberg RA. Lactate homeostasis and lactic acidosis. Ann Intern Med. 1980;92:227.
1-F. Metabolic Alkalosis
Chloride-Responsive (Urine Cl− <10 mEq/L)
Vomiting, nasogastric suction
Gastric drainage or fistula
Diuretics
Posthypercapnic state
Villous adenoma of colon
Congenital chloride diarrhea
Cystic fibrosis
Chloride-Resistant (Urine Cl− >20 mEq/L)
Primary aldosteronism
Secondary aldosteronism
Congestive heart failure
Cirrhosis and ascites
Malignant hypertension
Adrenocorticotropic hormone (ACTH) or glucocorticoid excess (Cushing disease, Cushing syndrome, ectopic ACTH production)
Bartter syndrome
Gitelman syndrome
Renin-secreting tumor (e.g., hemangiopericytoma)
Licorice ingestion
Excessive use of chewing tobacco
Severe potassium depletion
Congenital adrenal hyperplasia
Liddle syndrome
Miscellaneous
Administration of alkali or alkalinizing agents, especially in the presence of renal insufficiency:
Alkalinizing agents (e.g., citrate, lactate)
Antacids (milk-alkali syndrome)
Massive transfusion of blood or plasma substitute
Nonparathyroid hypercalcemia (e.g., bone metastases, multiple myeloma)
Nonreabsorbable anionic antibiotics, large doses (e.g., penicillin, carbenicillin)
Glucose ingestion after starvation
References
1. Shapiro JI, Kaehny WD. Pathogenesis and management of metabolic acidosis and alkalosis, p. 115. See Bibliography, 1.
2. Rose BD, p. 551. See Bibliography, 2.
1-G. Respiratory Alkalosis
Central Causes
Voluntary hyperventilation
Anxiety, pain
Hypoxia
Fever
Salicylate toxicity
Head trauma
Brain tumor
Central nervous system infection
Cerebrovascular accident
Pregnancy
Recovery phase of metabolic acidosis
Cardiopulmonary Causes
Congestive heart failure
Pneumonia
Pulmonary embolism
Interstitial lung disease
Adult respiratory distress syndrome
High altitude
Other
Hepatic insufficiency
Sepsis (especially gram-negative)
Drugs
Progesterone, medroxyprogesterone
Xanthines (e.g., aminophylline)
Catecholamines (massive amounts)
Nicotine
Mechanical ventilation
Heat exposure (e.g., heatstroke)
References
1. Rose BD, p. 673. See Bibliography, 2.
2. Kaehny WD. Pathogenesis and management of respiratory and mixed acid-base disorders, p. 154. See Bibliography, 1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree