Abdominoperineal Resection, Low Anterior Resection
Abdominoperineal and low anterior resections are performed for carcinoma of the rectum. Wherever possible, the anal sphincters are preserved and an end-to-end anastomosis done by low anterior resection or other, more complicated, sphincter-saving procedures. Neoadjuvant therapy significantly increases the rate of sphincter preservation. The emphasis in modern cancer surgery is on total mesorectal excision, which simply means sharp dissection carried as wide as possible, removing the fatty node-containing mesentery as an intact envelope around the rectum. In contrast, operations for benign disease such as ulcerative colitis are performed as close as possible to the rectal wall (see References at the end of the chapter).
SCORE™, the Surgical Council on Resident Education, classified abdominoperineal resection as a “COMPLEX” procedure and open partial colectomy as an “ESSENTIAL COMMON” procedure.
STEPS IN PROCEDURE
Position patient in lithotomy with access to both abdomen and perineum
Lower midline incision, explore the abdomen
Mobilize left colon by incising lateral peritoneal reflection, similarly incise peritoneum over right side, curving both peritoneal incisions down into pelvis where they continue anteriorly toward bladder or uterus
Identify both ureters, mobilize laterally in pelvis, and surround with silastic loops
Divide sigmoid with linear cutting stapler
Elevate sigmoid from pelvis and dissect sharply in presacral space
Clip any branches of middle artery as needed
Continue peritoneal incisions anteriorly over the posterior surface of the bladder (or uterus, in a female)
Male: Dissect in plane just posterior to seminal vesicles
Female: Excise portion of posterior vaginal wall if adjacent to tumor
Divide lateral attachments with clamps or clips
Assess feasibility of sphincter preservation
Abdominoperineal Resection
Complete dissection down to levator sling
Outline an elliptical incision
In male: Transverse perineal muscle forms anterior limit of dissection. In female: Continue to excise posterior wall of vagina
Divide posterior tissues until fascia anterior to coccyx is identified; divide this sharply to enter abdominal plane of dissection
Divide puborectalis muscles with cautery
Perform anterior dissection in male with care, identifying and preserving prostate
Pass specimen out through perineum and divide remaining anterior attachments
Fashion end sigmoid colostomy
Place closed suction drains and close perineal and abdominal wounds
Low Anterior Resection
Transect distal rectum with reticulating linear stapler and divide
Place two stay sutures on each side of rectal stump
Create purse-string suture in proximal sigmoid colon and insert anvil
Create end-to-end stapled anastomosis with EEA stapler passed transanally
Test anastomosis for leaks, reinforce if needed
Consider temporary diverting loop ileostomy if any difficulty has been encountered
Closed suction drains in pelvis
Close abdomen in usual fashion
HALLMARK ANATOMIC COMPLICATIONS
Injury to ureters
Injury to male urethra or prostate
Damage to pelvic autonomic plexus, causing impotence or ejaculatory problems in men
LIST OF STRUCTURES
Sigmoid colon
Rectum
Lateral rectal ligaments
Anal canal
Ureters
Bladder
Sacrum
Coccyx
Pelvic diaphragm
Levator Ani (Levator Sling)
Iliococcygeus muscle
Pubococcygeus muscle
Coccygeus muscle
Ischiorectal fossa
Pubic symphysis
Ischial tuberosities
Perineum
Anterior (urogenital) triangle
Posterior (anal) triangle
Anococcygeal raphe
Perineal body
Pudendal nerve
Pudendal (Alcock) canal
Aorta
Inferior Mesenteric Artery
Superior rectal (hemorrhoidal) artery
Middle rectal (hemorrhoidal) arteries
Internal Pudendal Artery
Inferior rectal (hemorrhoidal) arteries
Middle sacral artery
Common Iliac Arteries
Internal iliac arteries
Presacral venous plexus
Superior hypogastric plexus
In the Male
Prostate
Seminal vesicles
Membranous urethra
Bulb of penis
Rectovesical fascia (of Denonvilliers)
Rectovesical pouch
Transverse perineal muscles
In the Female
Uterus
Ovaries
Vagina
Rectouterine pouch (of Douglas)
In this chapter, abdominoperineal resection will be considered along with the closely related low anterior resection. Figure 101.1 shows the extent of resection, including wide excision of tissues surrounding the rectum. This dissection will be described as it is done for a male patient. The modifications necessary for a female patient are described at the end of this section. The corresponding laparoscopic procedures are described in Chapter 102e.
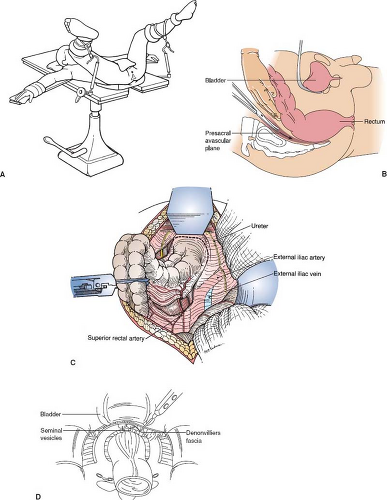
Position of the Patient and the Incision (Fig. 101.2)
Technical Points
Position the patient supine on the operating table. Use either specially constructed leg supports or homemade outrigger “skis” to support the legs in moderate abduction with mild flexion at the hips and knees (Fig. 101.2A). The buttocks should extend slightly over the end of the operating table. Comfortable access to the perineal region should be available for the operating surgeon. Avoid the use of standard lithotomy stirrups, because these produce excessive flexion at the hip and knee and have been associated with vascular complications when used for lengthy procedures. Close the anus securely with a purse-string suture. Prepare and drape the anterior abdomen and perineal region. Place a towel over the perineum to provide temporary coverage until access is required. The initial phase of the dissection is done through the abdomen, with the second assistant standing between the legs of the patient. The instrument nurse should stand on a stool. Do not proceed with the perineal dissection unless you are certain that sphincter preservation will not be possible.
A lower midline incision provides good exposure to the lower abdomen and pelvis. Make the incision from just above the umbilicus to the level of the pubis. Explore the abdomen. Mobilize the left colon as described in Chapter 81. Carry the peritoneal incisions anteriorly, about 1 cm up on the bladder, meeting in the midline between the bladder and the rectum.
Identify both ureters and surround them with Silastic loops. After the peritoneal incision has been completed and both ureters have been identified, divide the sigmoid colon at the point selected. Pass a hand behind the inferior mesenteric artery in the avascular plane just anterior to the vertebral bodies. Locate both ureters and confirm that they have not been included with the mesentery of the colon. Serially divide the mesentery of the colon with clamps. Using laparotomy pads, pack the proximal left colon up in the left upper quadrant.
The distal sigmoid is now completely free and can be circumferentially elevated from the pelvis, allowing access to the rectum. First, complete the posterior dissection. Elevate the sigmoid colon and initiate sharp dissection with Metzenbaum scissors in a plane just superficial to the sacrum (Fig. 101.2B). At the beginning of this dissection, you will see the aorta and common iliac vessels should be seen through a very light veil of areolar tissue. A few bands passing directly posterior between the colon and the presacral space can be divided using electrocautery or scissors. A middle sacral artery is usually present and should be secured with hemoclips. The colon should elevate easily, and a very thin glistening layer of retroperitoneal areolar tissue should be left intact over the presacral venous plexus. You should be able to dissect this plane easily by hand. If difficulty is encountered, it is possible that you are in the wrong plane; stop and reassess the situation. Torrential bleeding from the presacral venous plexus may follow inadvertent entry into this plexus. Conversely, remaining in the correct plane of dissection not only minimizes bleeding but also helps preserve autonomic nerves in the region. Dissection in the hollow of the sacrum should proceed readily until the tip of the coccyx is palpable and the rectosigmoid is elevated up on the hand. Check the hollow of the sacrum for hemostasis.
Next, turn your attention to the anterior dissection. Connect the peritoneal incisions laterally across the posterior surface of the bladder (Fig. 101.2C). Place three long hemostats, such as Crile hemostats, on the peritoneal reflection overlying the bladder. By sharp and blunt dissection, free the rectum from the posterior wall of the bladder until the seminal vesicles (in the male) are encountered (Fig. 101.2D). Carry this dissection down below the seminal vesicles, taking Denonvilliers fascia with the specimen. As noted in Figure 101.6, the posterior wall of the vagina is commonly excised with the specimen in a female. In this case, the anterior dissection need only proceed to a convenient point below the uterine cervix.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree