Abdominal Aortic Aneurysm Repair and Aortobifemoral Grafts
W. John. Sharp
Many aortic aneurysms are now repaired by an endovascular route. The classic open operation is still required in some circumstances. In this chapter, the anatomy of the abdominal aorta and iliac vessels is explored through the procedure of abdominal aortic aneurysm repair. The femoral region is then introduced through the closely related procedure of aortobifemoral bypass grafting.
Steps in Procedure
Abdominal Aortic Aneurysm Repair—Transperitoneal Approach
Midline incision from xiphoid to below umbilicus
Retract transverse colon cephalad
Reflect duodenum and small bowel cephalad and to the right
Reflect descending colon and sigmoid to the left
Preclot graft, if necessary
Isolate proximal and distal neck of aneurysm in preparation for clamping
Heparinize patient
Clamp aorta proximally and distally
Open the anterior wall of the aneurysm (longitudinal incision, T-ed across at superior and inferior ends)
Remove mural thrombus and suture-ligate any backbleeding lumbar vessels
Suture ligate the inferior mesenteric artery (from inside the aneurysm wall) if it is backbleeding
Suture graft to proximal aorta, using running suture
Flush and then clamp the graft distally; inspect suture line for leaks
Complete distal anastomosis and flush before opening clamps
Close the aneurysm sac over the graft after obtaining hemostasis
Abdominal Aortic Aneurysm Repair—Retroperitoneal Approach
Supine position with chest in right lateral decubitus position
Incision from tip of eleventh rib to midhypogastrium
Divide all muscular and fascial layers in the direction of the incision (not their fibers)
Mobilize the peritoneal sac medially to expose the aorta and both iliac vessels
Proceed as outlined above
Aortobifemoral Bypass
Expose femoral vessels by incision over each femoral pulse (inguinal ligament downward for approximately 10 cm)
Isolate and control the femoral arteries and branches
Create retroperitoneal tunnels over the anterial surface of the iliac and femoral arteries
Midline incision and exposure of the aorta as outlined above
Place clamp on proximal aorta, taking care not to fracture plaque
Clamp common, superficial, and profunda femoris arteries
Anastomosis to aorta can be performed as end (aorta) to end (graft) or as side (aorta) to end (graft)
Anastomosis to femoral vessels is end (graft) to side (vessel)
Obtain hemostasis and close
Hallmark Anatomic Complications
Left colonic ischemia from inadequate collaterals
Injury to ureters
Injury to left renal vein
Injury to hypogastric nerve plexus
Seroma (lymphocele) formation in groin incisions
List of Structures
Aorta
Left and right renal artery
Left and right gonadal artery
Inferior mesenteric artery
Lumbar arteries
Left and right common iliac artery
Left and right internal iliac (hypogastric) artery
Left and right external iliac artery
Left and right common femoral artery
Superficial circumflex iliac artery
Superficial epigastric artery
Superficial external pudendal artery
Profunda femoris artery
Medial femoral circumflex artery
Lateral femoral circumflex artery
Inferior Vena Cava
Left renal vein
Left and right common iliac vein
Left and right internal iliac vein
Left and right external iliac vein
Femoral vein
Profunda femoris vein
Hypogastric nerve plexus
Duodenum
Ligament of Treitz (suspensory muscle of the duodenum)
Ureters
External oblique muscle
Internal oblique muscle
Transversus abdominis muscle
Anterior rectus sheath
Rectus abdominis muscle
Inguinal ligament
Femoral sheath
Femoral triangle
Femoral Nerve
Cutaneous branch
Muscular branch
Genitofemoral nerve
Saphenous nerve
Adductor canal (of Hunter)
Abdominal Aortic Aneurysm Repair
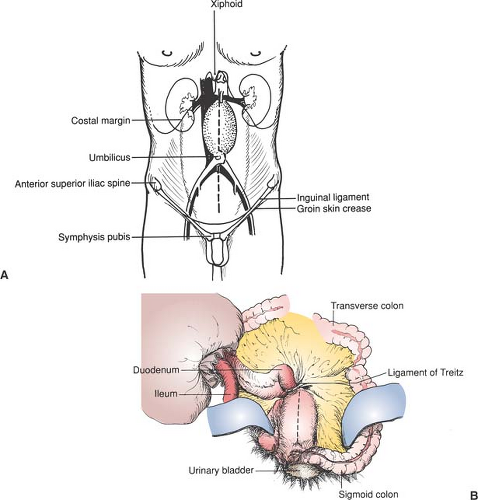
Skin Incision (Fig. 92.1)
Technical Points
Place the patient in a supine position, with a Foley catheter and appropriate monitoring devices in place. Prepare and drape the abdomen from the nipples to the knees. Cover the genitalia with a sterile towel. Secure all towels with iodophor-impregnated plastic adhesive drapes, rather than with sutures or towel clips. An antibiotic that is active against common gram-positive skin bacteria (e.g., a cephalosporin) is administered just before making the incision and for 24 hours postoperatively.
Most surgeons prefer a midline transperitoneal incision, as shown in Fig. 92.1, 92.2, 92.3 and 92.4. (An alternative retroperitoneal approach is presented in Fig. 92.5 and 92.6.) Extend the incision from the xiphoid to the midhypogastrium or below (Fig. 92.1A). Retract the transverse colon superiorly and divide the ligament of Treitz (suspensory muscle of the duodenum) to mobilize the duodenum to the right (Fig. 92.1B). Pack the small bowel into the right side of the abdominal cavity within a towel. Pack and retract the descending and sigmoid colon laterally and inferiorly if necessary. Self-retaining retractors such as the Omni are very helpful.
Anatomic Points
The midline incision has many anatomic advantages if a transperitoneal approach is used. In addition to providing maximal exposure of the peritoneal cavity, it affords a strong closure because several fascial and aponeurotic layers fuse as the linea alba. Retraction of the transverse colon superiorly displaces the transverse mesocolon superiorly, exposing the superior aspect of the root of the mesentery, which begins at the duodenojejunal flexure. Direct visualization and palpation of the ligament of Treitz (suspensory muscle of the duodenum) is then possible. This fibromuscular band arises from the right crus of the diaphragm and then passes posterior to the pancreas and splenic veins and anterior to the left renal vasculature. It may contain numerous small vessels. Reflection of the duodenum and small bowel to the right, and of the descending and sigmoid colon to the left, exposes the aneurysm, which is covered with parietal peritoneum.
Exposure of the Infrarenal Aorta and Iliac Arteries (Fig. 92.2)
Technical Points
Open the peritoneum over the aneurysm (Fig. 92.2A). Preserve as much of the hypogastric nerve plexus as possible because sexual dysfunction frequently results if these nerves are divided or devascularized.
In more than 90% of the cases, the superior neck of the aneurysm is below the origin of the renal arteries, where the left renal vein crosses the aorta. Exercise care to avoid injury to these vessels in dissecting the neck of the aneurysm for clamping. Rather than risk tearing the left renal vein during an unusually difficult exposure, it may be intentionally divided and ligated (preferably oversewn) to the right of the gonadal and adrenal branches to provide adequate, safe exposure with preservation of collateral drainage. The left renal vein may be retroaortic and thus highly susceptible to accidental injury and subsequent massive, difficult-to-control hemorrhage.
The ureters are also very near the aneurysm, and the potential for injury to these structures during dissection and retraction should be recognized. The ureters are most susceptible to
injury where they cross anterior to the iliac bifurcation to enter the pelvis. The common iliac veins are closely adherent to the arteries and should be carefully separated from them only for a distance that is sufficient to allow clamping of the arteries (Fig. 92.2B).
injury where they cross anterior to the iliac bifurcation to enter the pelvis. The common iliac veins are closely adherent to the arteries and should be carefully separated from them only for a distance that is sufficient to allow clamping of the arteries (Fig. 92.2B).
Aspirate blood from the inferior vena cava or aorta for preclotting of knitted Dacron grafts. (Preclotting of woven, “presealed” knitted, or PTFE grafts is unnecessary.) Then have the anesthesiologist administer heparin intravenously. Clamp all vessels gently to avoid dislodging atheroma or thrombus as emboli. Open the anterior wall of the aneurysm. At the superior and inferior necks of the aneurysm, extend the incision transversely in a T pattern through the anterior half of the wall. Leave the posterior portion intact for strong purchase of sutures. Remove mural thrombus and suture-ligate bleeding lumbar arteries. Retracting sutures or a self-retaining retractor placed in the wall of the aneurysm may be helpful. Remove any debris from both necks of the aneurysm.
If the inferior mesenteric artery is backbleeding, suture-ligate it from inside the aneurysm to avoid disturbing the collateral circulation to the distal inferior mesenteric artery. If there is concern regarding the viability of the colon at the conclusion of the procedure, reimplant the inferior mesenteric artery with a cuff of aortic wall into the graft. If the inferior mesenteric artery is not reimplanted, carefully inspect the bowel for signs of ischemia before closure of the abdomen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree