Key Points
Disease summary:
Recurrent pregnancy loss (RPL) is traditionally defined as three or more consecutive losses of recognized pregnancies in the first or early second trimester (<20 weeks of gestation). Sporadic spontaneous pregnancy loss occurs randomly in one-sixth of clinically recognized pregnancies. However, RPL must be distinguished from sporadic cases as these occasionally respond to treatment. Around 1% of couples attempting pregnancy experience RPL.
Hereditary basis:
Structural chromosomal abnormalities such as translocations and inversions are often identified in one partner of a couple experiencing RPL. The fetuses from these couples frequently carry chromosome copy number abnormalities which lead to miscarriage. Hereditary thrombophilia in females is also occasionally associated with RPL.
Differential diagnosis:
RPL is a heterogeneous condition. In addition to parental chromosomal abnormalities and hereditary thrombophilia, hormonal and metabolic disorders, uterine anatomic abnormalities, certain infections, and autoimmune disorders have been accepted as etiologic factors in RPL. However, up to 50% of these cases still remain unexplained after standard gynecologic, hormonal, and karyotypic investigations.
Diagnostic Criteria and Clinical Characteristics
RPL is traditionally defined as three or more consecutive losses of a recognized pregnancy in the first or early second trimester (<20 weeks of gestation).
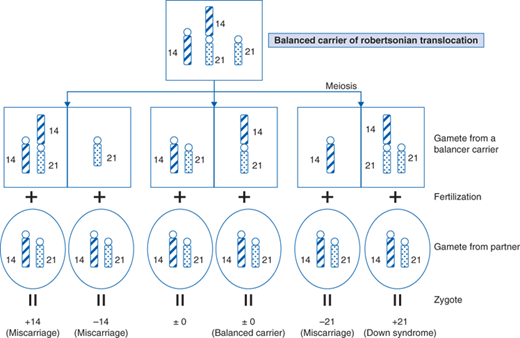
In 2% to 4% of couples experiencing RPL, a balanced structural abnormality is found in one partner. Chromosomal translocations are the most common structural abnormalities associated with early RPL. Robertsonian translocations involve the centric fusion of two acrocentric chromosomes (numbers 13, 14, 15, 21, and 22). Balanced carriers of Robertsonian translocations have no clinical symptoms, but often produce chromosomally unbalanced gametes. These numerical abnormalities in the autosome usually result in early fetal death, or occasionally in the birth of children with trisomy 13 or 21 (Fig. 99-1).
Figure 99-1
Chromosome Segregation in Balanced Translocation Carriers. Segregation of translocation and relevant chromosomes in balanced carriers for a t(14;21) Robertsonian translocation. Conceptuses are most often aneuploidy, resulting in miscarriage. Occasionally carriers give birth to a child with a normal or balanced karyotype, although some newborns are affected by trisomy 21.
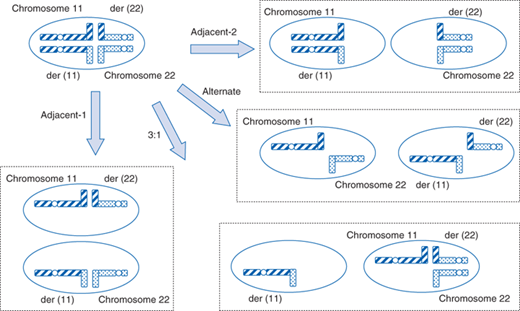
Other reciprocal translocations also cause RPL. During gametogenesis, paternal and maternal chromosomes undergo homologous pairing and recombine to segregate correctly in meiosis I. In balanced carriers of reciprocal translocations, normal and translocated chromosomes form an abnormal meiotic configuration that often leads to partially unbalanced gametes (Fig. 99-2). Large chromosomal imbalances result in fetal death, while chromosomally unbalanced children might be born if regions involved are small.
Figure 99-2
Meiotic Configuration During Gametogenesis in Balanced Translocation Carriers. Meiotic configuration during gametogenesis in balanced carriers of a t(11;22) reciprocal translocation. In adjacent 1 or 2, conceptuses harbor a partial trisomy and partial monosomy resulting in early pregnancy loss. Occasionally carriers give birth with a normal or balanced karyotype, while <1/10 newborns are affected by +der(22) syndrome (Emanuel syndrome) through a 3:1 segregation.
Other structural abnormalities such as inversions or insertions can also cause RPL.
Maternal endocrine and metabolic disorders occasionally contribute to the etiology of RPL. Females with diabetes mellitus, thyroid hormone disorders, and hyperprolactinemia are implicated as being at high risk of RPL. Luteal phase defects might possibly contribute to RPL through impaired placentation, but this is still controversial. Further, polycystic ovary syndrome is occasionally associated with RPL.
Uterine anatomic abnormalities are common causes of RPL, and 10% to 15% of females suffering from this disorder have congenital uterine abnormalities such as double uterus (bicornuate, septate, or didelphic). Uterine synechiae or fibroids may also be associated with RPL. Cervical incompetence is a well-known cause of midtrimester RPL. Its diagnosis is based on a history of late miscarriage preceded by spontaneous rupture of membranes or painless cervical dilatation.
Evidence has now accumulated that chorioamnionitis caused by ureaplasma species often contributes to late pregnancy loss. It is possible that females carrying such microorganisms might manifest RPL.
Thrombophilia, whether inherited or acquired, has been thought to contribute to a substantial percentage of RPL cases. It has been well documented that the hypercoagulation status in pregnant women preferentially causes pregnancy loss as a result of a placental thromboembolism. Protein C or S deficiency, antithrombin III deficiency, or activated protein C resistance are the common inherited causes of thrombophilia. Although such genetic susceptibilities to thrombophilia are more prevalent in women with late fetal losses, they are also a major cause of early miscarriage. The Leiden mutation (1691G>A) in the factor V gene or the PTm mutation (20210G>A) in the 3’UTR of the factor II (prothrombin) gene are also well-known risk factors for RPL in Caucasians, but these variants are rare in other populations. Recently, promoter polymorphisms for the annexin A5 gene have been reported to be associated with RPL (Table 99-1). Annexin A5 is a placental anticoagulant, and is decreased in the placentas of risk allele carriers. Antiphospholipid antibodies are a well-known cause of acquired thrombophilia and their presence often leads to a form of RPL known as antiphospholipid syndrome (see later).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree