Key Points
Disease summary:
Statins may cause a series of musculoskeletal and neuromuscular disturbances and diseases, including rhabdomyolysis and mild serum creatine kinase (CK) elevations. Genetic factors have been associated with an increased risk of statin-induced myopathy.
Statins or 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors are widely prescribed because of their cardiovascular benefits. Statins are well tolerated by most patients at low starting dosages but can produce statin-induced neuromyopathy and their usage is ultimately limited by toxicity.
The American College of Cardiology (ACC)/American Heart Association (AHA)/National Heart, Lung, and Blood Institute (NHLBI) definitions and terminology are widely used in the literature and therefore used here. They have defined four syndromes:
Statin myopathy (any muscle complaints related to statins)
Myalgia (muscle complaints without serum CK elevation)
Myositis (muscle complaints with CK elevation >10 ULN [upper limit of normal])
Rhabdomyolysis (CK activity >10-fold ULN with an elevated creatinine level consistent with brown urine and urinary myoglobin)
Muscle complaints encompass aches, cramps, pain, tenderness, weakness, fatigue, and heaviness and are broadly categorized as neuromuscular side effects (NMSEs).
NMSE occur in approximately 10% of patients during high-dose therapy, affecting compliance to therapy. NMSEs vary in extent among drugs and from patient to patient.
Increased serum CK activity provides the predominant means for assessing the degree of muscle injury, with elevation of CK activity to greater than 10-fold ULN suggested as indicating severe statin-induced neuromyopathy. Elevation of CK to greater than fourfold ULN with statin therapy may warrant testing for underlying metabolic muscle disease. However, serum CK activity correlates poorly with the more common and less severe NMSE, can be normal in patients with NMSE, and is not an effective clinical marker for common NMSE.
Differential diagnosis:
Muscle pain can be caused by bursitis, myofascial pain, muscle strain, osteoarthritis, radiculopathy, and tendonitis. Other etiologies for muscle complaints or an increased CK level are increased physical activity, trauma, falls, accidents, seizure, shaking chills, hypothyroidism, viral infections, carbon monoxide poisoning, polymyositis, dermatomyositis, alcohol abuse, and drug abuse (cocaine, amphetamines, heroin, or phencyclidine [PCP]).
Monogenic forms:
No single gene cause of NMSE is known to exist.
Family history:
One-third of the patients with myopathy have family members who also experienced symptoms associated with lipid-lowering drugs. The presence of family history almost doubles the risk of the adverse reaction.
Twin studies:
None available.
Environmental factors:
Physical exercise, addition of a new drug, or paradoxically, rest, or assuming the lying position may trigger symptoms. The disparate nature of these factors suggests more than one pathophysiology.
Genome-wide associations:
To date there exist two published genome wide studies of statin response. Severe statin myopathy has been strongly associated with the SLCO1B1 *5 variant.
Pharmacogenomics:
Statin efficacy (low-density lipoprotein-cholesterol [LDL-C] lowering, prevention of major adverse cardiovascular events) and the safety factors of NMSE and myositis strongly influence patient drug selection. Emerging studies are focused on predicting the balance of statin efficacy (LDL-C lowering, prevention of major adverse cardiovascular events) versus Safety.
Diagnostic Criteria and Clinical Characteristics
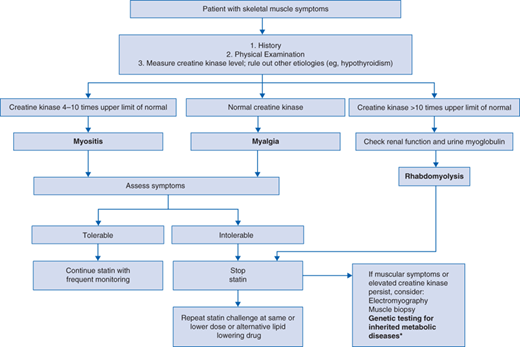
Diagnostic evaluation should include (see Fig. 9-1)
Assessment of family history to evaluate for predisposition to myopathy.
Physical examination focusing on tenderness to palpation and findings consistent with other causes of myopathy.
A CK level should be drawn and patients with elevated CK levels should be asked about recent strenuous exercise, significant alcohol, grapefruit or pomegranate juice ingestion, and the use of red yeast rice supplements or of medications that might interact with the statins. Also, a workup for other possible causes of myopathy should be initiated.
If the patient complains of brown urine or if CK levels are markedly elevated (>10 × ULN), renal function and urine myoglobin should be evaluated.
A muscle biopsy should be considered if the patient’s symptoms and/or the CK elevation persist after withdrawal of the lipid-lowering drug.
The clinical characteristics for statin-induced NMSE depend on the patient, ranging from myalgia, lassitude, and fatigue to frank proximal muscle weakness. Patients may experience an aching or cramping sensation in their muscles, nocturnal leg cramps, and tendon pain. Sensations may be widespread and increase with exercise, though paradoxically, some patients report sensations upon rest or lying down. Symptoms develop within 4 weeks to 4 years after initiation of statin therapy, and more often in response to high dose. The addition of a new drug can trigger myopathy.
The most frequent NMSE reported in 832 patients suffering statin-associated myopathy were heaviness, stiffness, and cramps in 57.9% of patients, and stiffness and cramps in 13.1% of patients. Most patients reported diffuse pain, but complaints focused on a given location, mostly in the lower limbs. Other symptoms were muscle weakness during physical activity and tendonitis, the latter reported by 24.4% of the patients. Most patients do not present with elevated CK activity.
Statins are used on a long-term basis and it is important to know which drugs may interact with them. Various medications may interact with statins, increasing serum concentrations and the risk of myopathy, rhabdomyolysis, and acute renal failure. Table 9-1 describes drug interactions and their prevention.
| Gene | Protein Function | Associated Medications | Polymorphisms | Frequency | Outcome |
|---|---|---|---|---|---|
| CYP2D6 | Cytochrome CYP450 metabolizing enzyme | Fluvastatin Atorvastatin, simvastatin | *3, *4, and *5 produce null activity | *3 and *5: 0.02 in European Caucasians *4: 0.1-0.2 in North Americans | *3, *5: higher incidence of fluvastatin intolerability in homozygotes *4: atorvastatin and simvastatin-induced myopathy |
| CYP3A5 | Cytochrome CYP450 metabolizing enzyme | Lovastatin, pravastatin, simvastatin, atorvastatin | *3 and *5 produce decreased activity | *3: Caucasian ~0.05 African >0.60 Asian 0.2-0.3 *5: not available | *3: homozygotes greater risk for muscle damage *5: elevated plasma concentration of simvastatin |
SLCO1B1 (OATP1B1) | Organic anion transporting polypeptide C which transports statins into hepatocytes | Simvastatin, pravastatin, atorvastatin, rosuvastatin, pitavastatin | *5 is associated with compromised hepatic uptake of the drug | 0.15-0.28 | Mild myopathy, serum CK ↑ Drug clearance ↓; plasma statin levels ↑ |
| ABCB1 | Intestinal P-glycoprotein efflux transporter | Atorvastatin, simvastatin | Various | Varied | Elevated plasma statin levels |
Screening and Counseling
Measurement of CK is a widely used screening diagnostic test for suspected muscle disease since it has relative predominance in skeletal muscle and is not falsely elevated by hemolysis. However, it may cause diagnostic uncertainty. Most symptomatic patients do not have elevated CK levels and an elevated level can be found in a patient mildly symptomatic or asymptomatic with respect to NMSE. Obtaining a pretreatment, baseline CK level is relatively inexpensive. It should be considered in patients who are at high risk of experiencing muscle toxicity, such as the elderly or when combining statin with an agent known to increase myotoxicity, or in patients suspected of carrying an inherited muscle disease (see Table 9-3). When measuring CK levels during statin therapy, clinicians should recognize that marked, clinically important CK elevations are rare and are usually related to physical exertion or other causes.
Currently genetic testing before or during the course of statin therapy is not part of clinical guidelines or physician practice.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree