Key Points
Disease summary:
The term thrombophilia refers to an inherited or acquired predisposition to thromboembolism.
Inherited thrombophilias include deficiencies of the three natural anticoagulant proteins antithrombin (AT), protein C (PC), and protein S (PS), and specific mutations in the genes for factor V (factor V Leiden) and prothrombin (prothrombin 20210G>A).
Inherited thrombophilias increase the risk for a first venous thromboembolism (VTE) 2- to 20-fold but are not major risk factors for arterial thromboembolism.
Although the risks vary, inherited thrombophilias are not strongly predictive of recurrent VTE after an initial episode.
The clinical expression of an inherited thrombophilia reflects a complex interplay between genetic and acquired risk factors.
Hereditary basis:
Deficiencies of the three natural anticoagulant proteins AT, PC, and PS are typically inherited as autosomal dominant traits. However, rare homozygous or compound heterozygous patients have been reported and they have a much more severe phenotype.
Mutations in the factor V Leiden and prothrombin 20210G>A predispose to thrombophilia both in the heterozygous and homozygous states but the latter tends to confer higher risk (see later).
Differential diagnosis:
The differential diagnosis of VTE includes multiple inherited and acquired thrombophilic disorders.
Because these disorders are clinically indistinguishable, laboratory testing is required for diagnosis in each case.
Acquired thrombophilias include antiphospholipid antibodies, high levels of several clotting factors (factors VIII, IX, XI), myeloproliferative disorders and paroxysmal nocturnal hemoglobinuria (PNH).
Homozygosity and compound heterozygosity for two common polymorphisms in the 5,10-methylenetetrahydofolate reductase (MTHFR) gene (C677T, A1298C) predispose to mild hyperhomocysteinemia. MTHFR polymorphisms do not increase the risk for VTE independent of homocysteine levels and genetic testing is not recommended.
Diagnostic Criteria and Clinical Characteristics
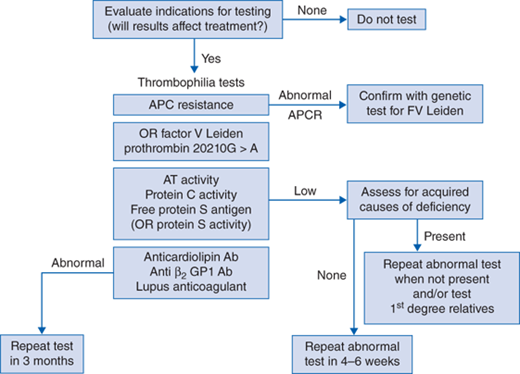
At least one of the following (Fig. 18-1)
Identification of factor V Leiden or prothrombin 20210G>A mutation
Abnormal activated PC (APC) resistance assay confirmed by a genetic test for factor V Leiden
Low AT activity
Low PC activity
Low free PS antigen (and/or PS activity)
The diagnosis of AT, PC, or PS deficiency also requires
Exclusion of acquired causes of a deficiency
Repeat testing on a separate sample to confirm a low protein level
Demonstration of a deficiency in family members in difficult cases
Thrombophilia testing should include tests for inherited and acquired disorders (Table 18-1):
| Diagnosis | Gene Symbol | Test Method | Mutation | Factors Affecting Testing |
|---|---|---|---|---|
| Factor V Leiden | F5 | Targeted mutation analysis | 1691G>A | Reliable during acute VTE, DIC, liver disease, warfarin, heparin |
| Prothrombin 20210G>A | F2 | Targeted mutation analysis | 20210G>A c.*97G>A | Reliable during acute VTE, DIC, liver disease, warfarin, heparin |
| Antithrombin deficiency | SERPINC1 | Antithrombin activity | >200 reporteda | ↓ by acute VTE, heparin, DIC, liver disease |
| Protein C deficiency | PROC | Protein C activity | >160 reporteda | ↓ by Vit K def., warfarin, acute VTE, DIC, liver disease |
| Protein S deficiency | PROS1 | Free protein S antigen (or protein S activity) | 300 reporteda | ↓by Vit K def., warfarin, acute VTE, DIC, liver disease, estrogen, pregnancy, inflammation |
APC resistance or DNA assay for factor V Leiden
DNA assay for prothrombin 20210G>A
AT activity
PC activity
Free PS antigen
Immunoassays for anticardiolipin and beta-2-glycoprotein-1 antibodies
Multiple coagulation tests for a lupus inhibitor.
Measurement of homocysteine is discouraged since lowering levels with vitamin supplements does not reduce thrombotic risk. Clotting factor levels (eg, factor VIII, factor IX) are not routinely included since the cutoff values for identifying high-risk individuals are not well defined.
The APC resistance assay is a partial thromboplastin time (PTT)-based screening test with almost 100% sensitivity and specificity for the factor V Leiden mutation. The DNA test is required to confirm a positive screening assay, and to distinguish heterozygotes and homozygotes. Molecular genetic tests for factor V Leiden and prothrombin 20210G>A are not affected by acute thrombosis, illness, or antithrombotic agents.
Functional assays of AT and PC activity detect both quantitative and qualitative defects. The PS activity assay is less reliable but is useful to confirm the diagnosis and detect rare qualitative defects Anticoagulant protein levels may be temporarily reduced by acute thrombosis, disseminated intravascular coagulation (DIC), surgery, liver disease, and nephrotic syndrome. Testing is optimally performed several months after an acute VTE episode when the patient is not on anticoagulation. Therapeutic dose heparin can reduce AT levels by up to 30%. Proteins C and S levels are lowered by vitamin K deficiency and warfarin therapy. PS levels fall during pregnancy, estrogen contraception, and acute or chronic inflammation. Testing should be delayed for at least 2 to 3 weeks after stopping warfarin, and several months after delivery or discontinuation of estrogen.
The primary clinical manifestation of inherited thrombophilia is VTE (deep venous thrombosis [DVT] and pulmonary embolism). DVT usually involves the legs but also occurs in upper extremities. Less commonly, thrombosis develops in unusual locations such as cerebral, hepatic, portal and renal veins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree