Key Points
Disease summary: Psoriasis and psoriatic arthritis (PsA) are complex genetic disorders involving multiple genes and epigenetic factors that contribute to disease manifestation and progression.
Typical psoriasis lesions are well demarcated, scaly erythematous plaques that occur in various sizes and shapes. Psoriasis most often manifests on the extensor surfaces of the elbows and knees, as well as the scalp and sacral lesions.
PsA is an inflammatory arthritis associated with psoriasis. Approximately 30% of patients with psoriasis will at some point develop psoriatic arthritis. The psoriasis precedes the onset of arthritis in approximately 70% of patients, occurs concurrently in 15% of patients, and follows the onset of psoriasis in the remaining 15% of patients.
The diagnosis of PsA is dependent on clinical, laboratory, and radiologic assessments. The recently published classification criteria, ClASsification criteria for Psoriatic ARthritis (CASPAR) is now widely accepted for classifying this entity.
Differential diagnosis:
The differential diagnosis of psoriasis includes atopic dermatitis, contact dermatitis, pityriasis rosea, pityriasis alba, seborrheic dermatitis, nummular eczema, and lichen planus. The differential diagnosis for PsA includes rheumatoid arthritis, ankylosing spondylitis, Reiter syndrome, inflammatory bowel disease (IBD) arthropathy, and systemic lupus erythematous.
Monogenic forms:
There are no monogenic forms for psoriasis and PsA. The genes associated with psoriasis and PsA appear to be multiple with each displaying modest effect size.
Family history:
An affected first-degree relative confers a relative risk between 4 and 10 for psoriasis. PsA displays stronger heritability than psoriasis, as an affected first-degree relative confers a relative risk between 30 and 47.
Twin studies:
Twin studies in psoriasis demonstrate that there is a threefold increase in concordance in monozygotic versus dizygotic twins. The one twin study in PsA did not reveal significant heritability.
Environmental factors:
Trauma, streptococcal infection or HIV infection may precipitate or worsen psoriasis and PsA.
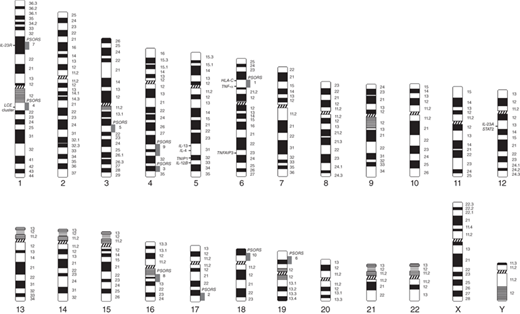
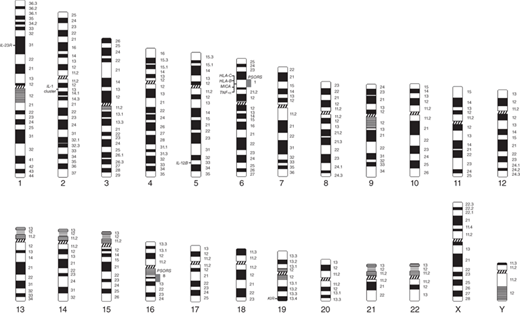
Genome-wide associations: Numerous genes are associated with the pathogenesis of both psoriasis and PsA (Tables 106-1 and 106-2; Figs. 106-1 and 106-2).
Pharmacogenomics:
Polymorphisms exist that affect the pharmacokinetic and pharmacodynamic profiles of many drugs used in the treatment of psoriasis and PsA (Table 106-3). Pharmacogenetic data specific to psoriasis and PsA are lacking.
Figure 106-1
Location of genes and loci associated with risk for psoriasis. Abbreviations: HLA, human leukocyte antigen; IL, interleukin; TNF-α, tumor necrosis factor-α; TNFAIP3, TNF-α-induced protein 3; TNI P1, TNFAIP3 interacting protein 1; LCE, late cornified envelope; STAT2, signal transducer and activator of transcription 2; PSORS; psoriasis susceptibility.
Figure 106-2
Location of genes and loci associated with risk for psoriatic arthritis. Abbreviations: HLA, human leukocyte antigen; IL, interleukin; TNF-α, tumor necrosis factor-α; MIC A, major histocompatibility complex class I-related gene A; KIR, killer inhibitory receptor; PSORS; psoriasis susceptibility
| Gene/Locus | Chromosome Location | Variant | Function |
|---|---|---|---|
HLA-C | 6p21.3 | rs12191877 rs10484554 rs2395029 | Antigen presentation |
IL-12B | 5q33.3 | rs3212227 rs6887695 rs2082412 rs3213094 | Stimulates growth and differentiation of Th1 or Th2 cells; stimulates the production of IFN-γ and TNF-α from T and NK cells |
IL-23R | 1p31.3 | rs7530511 rs11209026 rs11465804 rs12131065 rs2201841 | Receptor for the proinflammatory cytokine, IL-23, which stimulates IFN-γ production, proliferation of memory Th1 cells, and has a role in the novel Th17 pathway |
IL-23A/STAT2 | 12q13.2 | rs2066808 | Stimulates IFN-γ production, proliferation of memory Th1 cells, and has a role in the novel Th17 pathway |
TNFAIP3 | 6q23.3 | rs610604 | Regulates TNF-α-induced NFκB activation reducing inflammation |
TNIP1 | 5q32-33.1 | rs17728338 | Regulates TNF-α-induced NFκB activation reducing inflammation |
IL-13/IL-4 | 5q31 | rs20541 rs848 | Involved in B-cell differentiation and Th2 differentiation and function |
LCE gene cluster | 1q21 | rs6701216 rs4085613 | Involved in epidermal differentiation |
| Gene/Locus | Chromosome Location | Variant | Function |
|---|---|---|---|
HLA-C | 6p21.3 | rs10484554 rs2395029 | Antigen presentation |
TNF-α | 6p21.3 | −238G>A in promoter region | A cytokine involved in inflammation, immune response regulation, and apoptosis |
MICA | 6p21.3 | MICA*002 | Functions as a stress-induced antigen recognized by NK cells, NKT cells, and most of the subtypes of T cells |
IL-12B | 5q33.3 | rs6887695 rs3212227 | Stimulates growth and differentiation of Th1 or Th2 cells; stimulates the production of IFN-γ and TNF-α from T and NK cells |
IL-23R | 1p31.3 | rs11209026 | Receptor for the proinflammatory cytokine, IL-23, which stimulates IFN-γ production, proliferation of memory Th1 cells, and has a role in the novel Th17 pathway |
IL-1 gene cluster | 2q13 | rs3811047 | A potent proinflammatory cytokine, involved in immune responses and inflammatory processes |
KIR2DS1/KIR2DS2 (+ HLA-Cw*0602) | 19q13.4 | CNV | Located on NK cells and recognizes antigen-presenting molecules; produce large quantities of cytokines (IL-1, TNF-α) |
| Gene | Associated Medications | Goal of Testing | Variants | Genotype/Phenotype Correlation |
|---|---|---|---|---|
CYP2C9 | NSAIDs | Safety and efficacy | *2, *3 | Increased risk of gastrointestinal bleeding; lower dose required |
SLC19A1 | Methotrexate | Safety and efficacy | 80G>A | Uptake lowest in individuals with GG genotype than those with GA or AA genotypes |
TYMS | Methotrexate | Efficacy | Tandem repeat | Alleles with only 2 repeats associated with improved response; alleles with 3 repeats associated with MTX resistance |
MTHFR | Methotrexate | Safety | 677C>T | CT/TT genotype associated with increased ADRs and higher rate of MTX toxicity |
MTHFR | Methotrexate | Safety | 1298A>C | AC/AA genotype associated with higher rate of MTX toxicity; lower dose required |
ATIC | Methotrexate | Safety | 347C>G | GG genotype associated with ADRs |
DHODH | Leflunomide | Efficacy | 19C>A | Frequency of remission increased with C allele |
CYP1A2 | Leflunomide | Safety | *1F | CC genotype associated with a higher rate of toxicity; lower dose required |
TPMT | Azathioprine | Safety and efficacy | *2, *3A, *3C | Variants associated with decreased efficacy and increased toxicity; lower dose is required |
NAT2 | Sulfasalazine | Safety | *4 | Decreased risk of severe ADRs |
TNF-α | Etanercept Infliximab | Efficacy |