Figure 17-1. National immunization survey of teens, United States, 2006 to 2013. ACIP, Advisory Committee on Immunization Practices; HPV, human papillomavirus; MenACYW, meningococcal conjugate; Tdap, tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis. (Reproduced from Centers for Disease Control and Prevention (CDC). National and state vaccination coverage among adolescents aged 13-17 years—United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(34):685-706.)
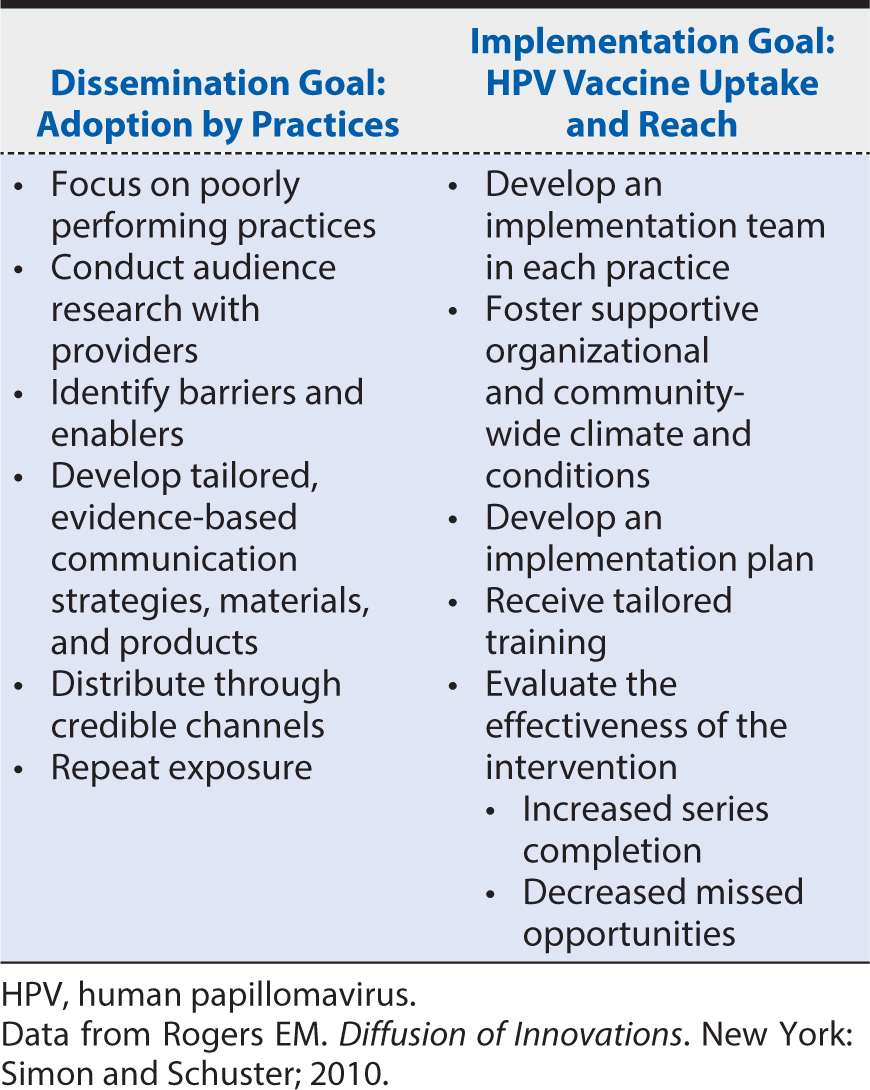
Systematic reviews and dissemination research show that active, multifaceted dissemination strategies are more effective than passive strategies for changing provider behavior. Educational outreach, academic detailing, and the use of local opinion leaders are the most consistently effective interventions reported. Implementation strategies likely to work best in primary care and among PHCP include academic detailing and quality improvement approaches. Table 17-1 describes evidence-based goals and strategies for both D & I approaches to address deficits in HPV vaccination rates.
Table 17-1. Dissemination and implementation goals and strategies for increasing human papillomavirus vaccination rates.
OVERVIEW: IMPLEMENTATION SCIENCE
This chapter is structured to acquaint the reader with the growing and emerging field of implementation sciences (IS), the study of methods to promote the integration of research findings and evidence into health care policy and practice. IS seeks to understand the behavior of health care professionals and other stakeholders as a key variable in the sustainable uptake, adoption, and implementation of evidence-based interventions.
As a newly emerging field, the definition of IS and the type of research encompassed by it may vary according to setting and sponsor. However, the intent of IS and related research is to investigate and address major bottlenecks (e.g., social, behavioral, economic, management) that impede effective implementation, test new approaches to improve health programming, and determine a causal relationship between the implementation intervention and its impact.
We present the rationale and need for IS along with definitions, outcomes, and constructs that place IS within both the translational continuum and the broader framework of D & I research. We also present theories and models used in D & I research. The earlier scenario presents an example of how D & I and especially IS can be applied to a pressing public health concern: increasing delivery of the HPV vaccine among adolescent females and males.
INTRODUCTION: RATIONALE AND NEED FOR IMPLEMENTATION SCIENCE
Over the past 25 years, we witnessed great strides in biomedical knowledge, including our understanding of basic biologic processes and the pathophysiology of disease, the development of interventions to prevent and treat disease, and the creation of evidence-based guidelines to support health and health care practice. Despite these efforts and the possibility of even more exciting discoveries in the near term, we have not realized the tremendous potential for impact and benefit of these dramatic therapeutic innovations on the management and cure of previously fatal diseases and on the prevention of conditions contributing to serious health consequences.
American health care falls short of care in other developed countries based on measures of quality, outcomes, costs, and equity. One reason for this paradox is that the results of many research studies are never translated into meaningful changes in patient care. By some estimates, it takes 15 to 20 years for many new interventions to become part of usual care, and this “implementation gap” prevents the public from experiencing timely benefits from the resources invested in research and can needlessly prolong suffering. A report by the Institute of Medicine commented on the remarkable disconnect between medical research and practice, noting that scientific knowledge about best care is not systematically applied. The report estimated an average of 17 years for 14% of knowledge generated by clinical trials to be incorporated into practice, and even then application is not uniform. The committee recommended that the U.S. government establish a comprehensive program aimed at making scientific evidence more useful and more accessible to clinicians and patients.
Delays in assembling, disseminating, and implementing scientific evidence to support the use of proven health and health care interventions and practices and the discontinuation of interventions with little or no evidence of efficacy are particularly problematic for the U.S. health care system given increasing financial and regulatory incentives and mandates promoting a shift toward evidence-based practice. Findings from clinical, health services, and comparative effectiveness studies—especially as assembled for systematic reviews and similar documents—need to be communicated and disseminated effectively to influence optimal and timely practice and health policy implementation. A growing emphasis on effective D & I science is developing in response to this evidence-to-practice gap.
D & I science seeks to understand how to systematically facilitate the utilization of evidence-based approaches to improve the quality and effectiveness of health promotion, health services, and health care. Barriers to D & I can arise at multiple levels in our complex health care delivery system, including the patient, health care provider, organization, market, and policy levels.
DEFINITIONS, OUTCOMES, AND CONSTRUCTS
There are no fixed and universally accepted definitions of evidence, IS, implementation, or implementation research. Furthermore, these terms are often combined or confused with diffusion, dissemination, and dissemination research. This ambiguity creates confusion among health care providers and other users of scientific evidence as well as challenges for D & I researchers seeking to expand the evidence base for this emerging field.
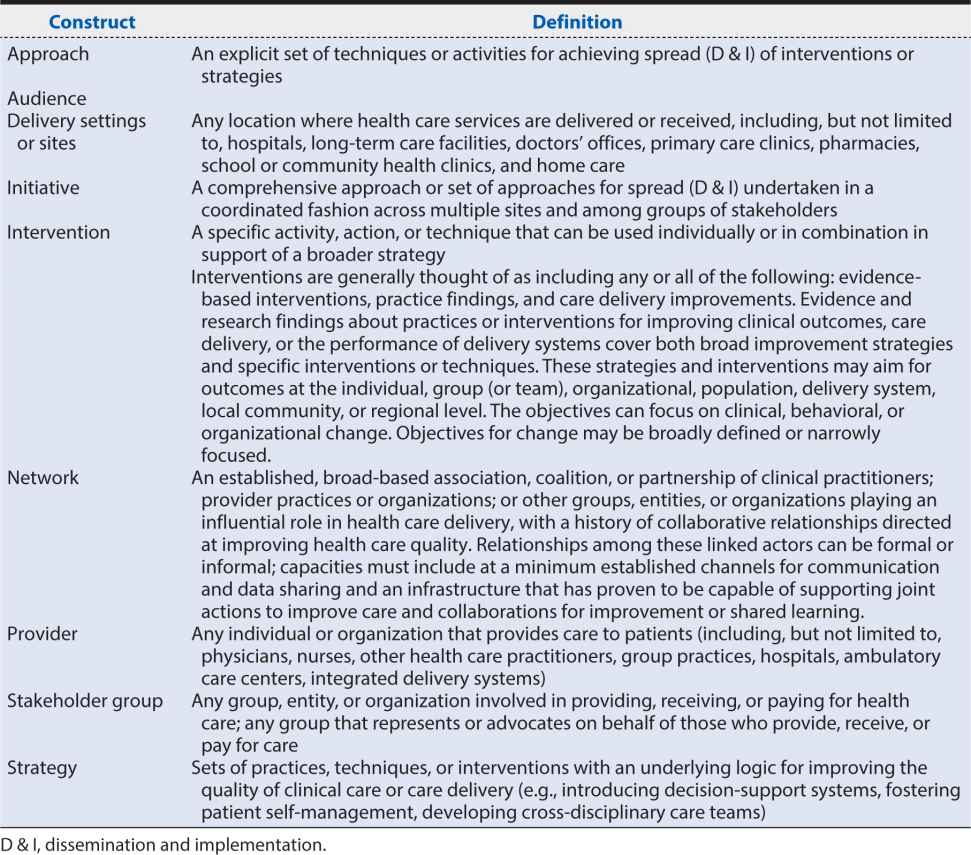
We present definitions for selected terms from widely recognized and accepted sources and recent reviews of D & I research. We suggest that intention and outcome-based constructs for choosing among these terms depends on the purpose of the work, the intended audience, and expected outcome(s) (Table 17-2). Regardless of the specifics associated with each definition of D & I, the expected outcome or intent of the activities described for each definition distinguishes it from the other. We further define constructs of D & I approaches used primarily with health and health care stakeholders in various settings to advance the awareness, adoption, use, and impact of health and health care evidence, information, and interventions (Table 17-3).
Table 17-2. Dissemination and implementation definitions and outcomes.
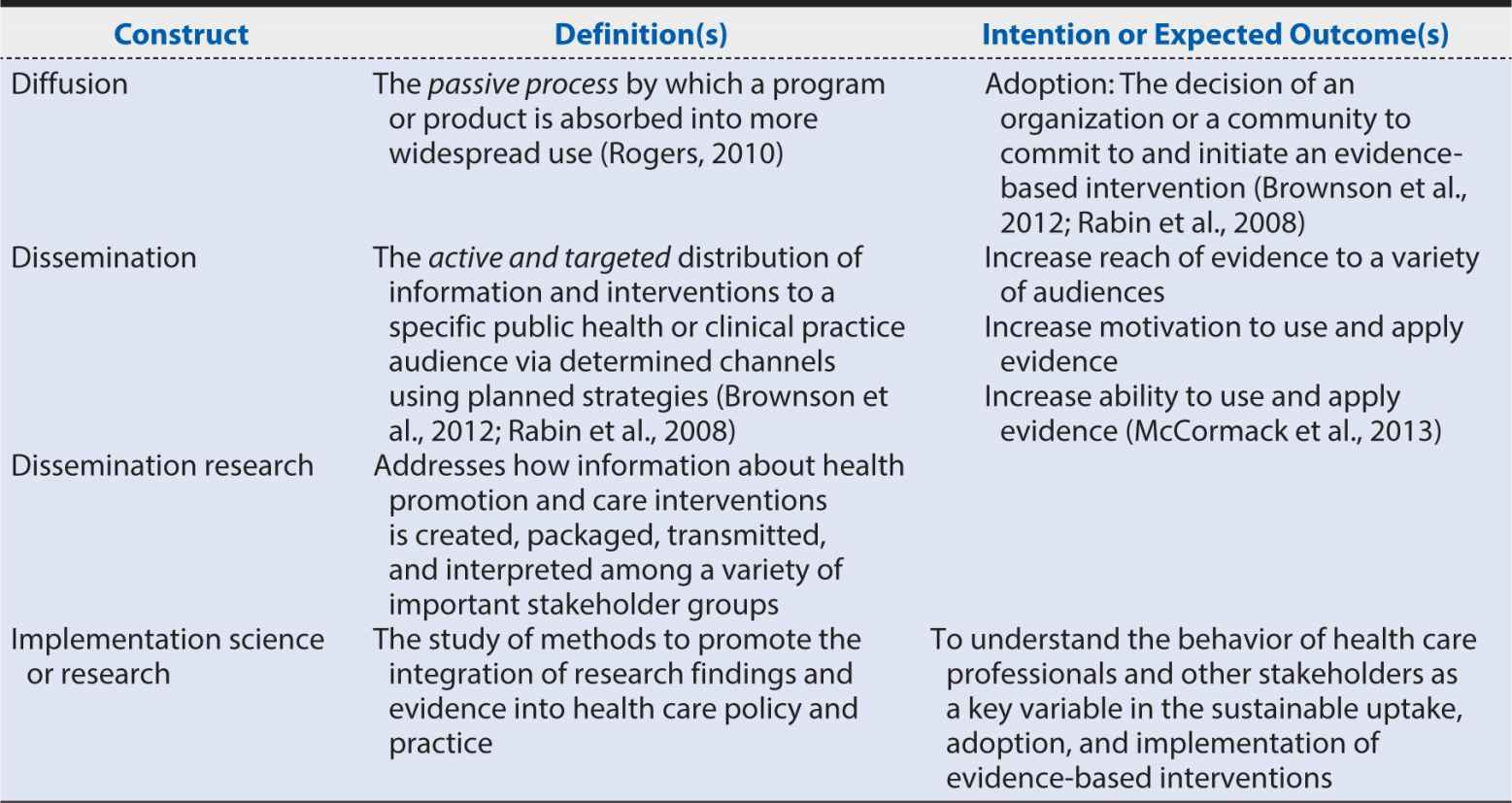
Table 17-3. Constructs and definitions.
Evidence
We use a recently suggested definition of evidence: data that have been assembled, reviewed, and presented by evidence developers and that have been used to make recommendations. Evidence may be assembled from the peer-review literature, gray literature, or a combination of both. Included studies may be randomized controlled trials (RCT), observational studies, or practice-based evidence reported in the peer reviewed literature or elsewhere (e.g., gray literature). Evidence about nonclinical interventions often derives from the social, behavioral, and management sciences. Because findings from single research studies are usually insufficient to guide practice and behavior change, most evidence is created using systematic review processes, including meta-analysis.
Systematic reviews are undertaken on a wide range of health and health care topics by a number of organizations and groups including the United States Preventive Services Task Force (USPSTF), The Community Guide to Preventive Services (Community Guide), the Agency for Healthcare Research and Quality (AHRQ) Evidence-based Practice Center (EPC), the Cochrane Collaborative, and professional and other organizations. Evidence resulting from these reviews may be biased by the type of review method(s) used, by the framing of specific key questions to be answered by the review, by the types of literature included in the review, by conflict of interest among those undertaking and endorsing or soliciting the review, and by temporal effects.
The most robust evidence is based on comparisons of two or more approaches designed and tested via RCT to achieve the same goal although current practice or usual care is often one of these approaches. For example, information about the efficacy of one drug compared with another drug for a specific indication such as pain relief may be evaluated based on studies evaluating harm (e.g., adverse events, addictive properties) and benefit (e.g., magnitude of expected effect or pain relief) associated with each drug. Because systematic review findings are often unequivocal or hampered by inconsistent study designs and outcomes, most review processes include a means of achieving consensus among experts and stakeholders about review findings and how those findings inform our understanding of intervention(s) to affect change in health or health care. Mechanisms for involvement of experts and stakeholders vary depending on the sponsor of the review but generally include periodic involvement of these individuals in all phases of a systematic review and, in particular, phases requiring decisions about review design, specification of key questions for the review, review findings, and interpretation of findings.
Dissemination
Dissemination is described in many ways (see Table 17-2) but in most instances refers to the active and targeted distribution of evidence, information, or interventions via determined channels using planned strategies to a specific public health or clinical practice audience. In contrast to diffusion, which is a passive, informal process, dissemination is a formal, planned process with the intent of spreading knowledge and associated evidence-based interventions to stimulate adoption and enhance the integration of the evidence, information, or intervention (or combinations of these) into routine practice. Dissemination has been characterized as a necessary but not sufficient antecedent of adoption and implementation of evidence.
Dissemination Outcomes
Existing dissemination models and approaches identify several very broad goals or outcomes for the dissemination of evidence and information. We focus on three intended goals of dissemination:
1. Increase reach to a variety of audiences: Reach is defined as the absolute number, proportion, and representativeness of individuals who are willing to participate in a given initiative. Approaches for increasing reach include distributing evidence, information, or interventions widely to intended audiences and across many settings using appropriate channels of communication and dissemination, including postal and electronic mail and electronic or digital, social, and mass media. Common metrics to measure increased reach among members of a target audience include increases in:
a. The proportion of audience members indicating awareness of the evidence or able to adequately describe the evidence, its components and source(s)
b. The range of media and other exposure to the evidence within geographic or certain population groups or practice settings
2. Increase motivation to use and apply such information: Motivation is defined as increasing audience member interest in using and applying the evidence, information, or interventions in their practice settings. Frequent strategies to increase motivation to use and apply evidence include the use of experts, champions (also known as a cheerleader), opinion or thought leaders, or social networks.
3. Increase ability to actually use and apply evidence: This includes providing additional resources in terms of the evidence, information, or interventions, such as how it can be incorporated into current practice or specific suggestions for change, to enhance a traditional dissemination strategy (e.g., by also providing additional resources or information; skills-building efforts).
It is also common practice to combine multiple dissemination strategies (often labeled as multicomponent strategies) to address a combination of reach, ability, or motivation goals. Several recent reviews indicate that multicomponent strategies are in fact the most efficacious and effective approaches to achieve dissemination goals and outcomes. For example, to alleviate the health effects of secondhand smoke exposure, the Centers for Disease Control and Prevention (CDC), the Legacy Foundation, and other professional and advocacy organizations use multicomponent dissemination strategies such as small and mass media, testimony, and in-person presentations by opinion leaders and celebrities and skills-building activities to increase the numbers of individuals and organizations who are aware of the dangers of secondhand smoke exposure and who are motivated to use and apply this evidence to change smoke-free environment policy and legislation in a variety of settings.
Dissemination Research
Dissemination research addresses how evidence, information, and interventions to promote and improve health and health care are created, packaged, transmitted, and interpreted among a variety of important stakeholder groups. For example, a study might explore the effectiveness of various combinations of strategies to deliver tailored and targeted messages about evidence. Strategies could include different media channels (e.g., print, Internet, radio or TV or other mass media, face-to-face interactions, or social media). Effectiveness could be evaluated via comparisons of outcomes associated with each dissemination strategy such as intervention reach, adoption, or use in the target audience.
Implementation
Implementation has been defined as the use of strategies to integrate evidence-based health interventions and change practice patterns within specific settings. Alternate forms of this definition (see Table 17-2) offer slight variations on this theme by asserting that implementation also involves adoption or integration of evidence-based interventions and strategies by individuals, sites, and organizations within specific settings. Implementation is often seen as a step after successful completion of dissemination strategies. The intent of implementation strategies is to address major, identified bottlenecks (e.g., social, behavioral, economic, management) that impede effective implementation and test new approaches to improve health programming, as well as determine a causal relationship between the implementation intervention and its impact. The evidence base for implementation strategies and interventions is empirical documentation of sufficient strength, clarity, and technical merit to produce strong expectations as to the likelihood of success in achieving improvement goals.
Implementation Outcomes
Implementation outcomes include the actual, documented use or integration of the intervention or innovation by the intended users into their practice, community, or academic setting. For example, the Treating Tobacco Use and Dependence Guidelines from the USPSTF have been widely disseminated and support the efficacy of pharmacologic and behavioral approaches for helping patients to quit using tobacco. Treatments are specified for all smokers and for different categories of smokers, such as pregnant women, hospitalized patients, and those with multiple comorbidities. Although physicians may be aware of efficacious treatment options recommended for smoking cessation, recommended approaches for assessing and treating patient tobacco use are often not undertaken for a variety of reasons specific to their organizations or sites and to individual practitioners such as not being aware of the evidence, time constraints affecting use of the evidence, or self-efficacy regarding implementation of evidence. Successful implementation of methods to assess tobacco use status could be established via electronic health record (EHR)–based practitioner prompts to assess and record tobacco use status for each patient at every visit. This achievement would establish tobacco use as a vital sign on par with other practices such as blood pressure measurement and indicate successful, universal implementation of one part of a treatment guideline. Continuing to pursue other components of the recommended tobacco treatment strategy such as assessing willingness to quit using tobacco, offering assistance in quitting, and arranging appropriate referral and follow-up might require the use of different implementation strategies to achieve universal delivery of each component.
Implementation Science
Implementation science (or research) is the study of methods and strategies to promote the integration of research findings and evidence into health care policy and practice. It seeks to understand the behavior of health care professionals and other stakeholders as a key variable in the sustainable uptake, adoption, and implementation of evidence-based interventions. For example, primary care clinicians generally have little time available to help their patients quit smoking cigarettes. To reduce the barrier associated with clinician time, several options are recommended by the current guidelines, including the use of reminders, EHR prompts, and less time-intensive approaches such as the 3 As + R method (ask, advise, assess, and refer). In addition to assessing differences in “effect” of each of these strategies, IS would also attempt to determine if one approach compared with another would be more likely to (1) be implemented (e.g., process outcome), (2) achieve cessation for tobacco users (e.g., behavioral or clinical outcome), or (3) to be preferred by either practitioners or patients.
Implementation science and research tools and approaches often used to undertake the development and assessment of alternate implementation strategies include qualitative research methods to identify bottlenecks and underlying determinants from varying perspectives, continuous quality improvement measures and methods, performance monitoring, and assessments of patient and clinician satisfaction.
DISSEMINATION AND IMPLEMENTATION RESEARCH THEORIES AND MODELS
Although this discussion focuses on health promotion, health services and health care, much of the work to date in D & I science and practice stems from other industries and disciplines, including agriculture, public health, organizational behavior, psychology, political science, and marketing. Because of the interdisciplinary nature of implementation research, it is important to organize and synthesize models and frameworks from a broad perspective to better understand overlapping constructs and establish a framework for moving the field forward.
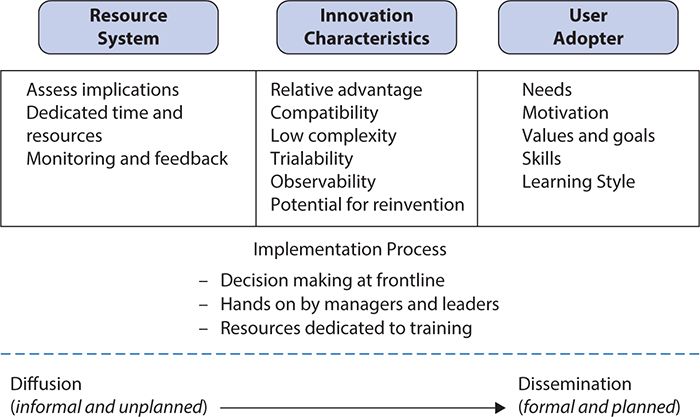
A recent review of the use of theory in D & I research found that only 53 of 252 studies reviewed used theories, and a small number of theories accounted for the majority of theory or model use, including PRECEDE (Predisposing, Reinforcing, and Enabling Constructs in Educational Diagnosis and Evaluation), diffusion of innovations, information overload, and social marketing (academic detailing). All models acknowledge the complex variables that can influence D & I. Greenhalgh and colleagues (2004) emphasize characteristics of the innovation itself and of the adopters of the innovation (either as individuals or as a system) along with the adoption process as critical in determining implementation success. As such, the interaction among the innovation, the proposed adopter(s), and the context determines the success of dissemination and implementation strategies (see Figure 17-2).
Figure 17-2. Factors impacting dissemination and implementation of innovation.
In terms of innovation or intervention characteristics, those more likely to be adopted and implemented have a clear and unambiguous advantage for the individual and system and are compatible with adopter values and norms; are feasible, workable, and easy to use; have proximal, observable benefits; and can be tried on a limited basis before adoption. Important prerequisites for adoption include awareness of the intervention or innovation by intended adopters, the availability of sufficient information or training in its use, and clarity about how the intervention or innovation will impact users personally. Because successful individual adoption is only one component of implementation in organizations, critical advances are also needed in the field to understand and evaluate system readiness and specific implementation strategies and processes. Studies to date suggest that if a large organization is mature, functionally differentiated (divided into departments or units) with decentralized decision-making structures and dedicated time and resources for innovation, it is more likely to be successful in implementing interventions. Nonstructural determinants of organizational readiness include the absorptive capacity for new knowledge (i.e., do the staff have the skills and time available to consider and use the innovation or intervention?) and the receptive context for change, including strong leadership, strategic vision, and good managerial relationships.
Other systematic reviews and dissemination research show that active dissemination strategies are more effective than passive strategies, and active multifaceted approaches are most effective for changing provider behavior. Educational outreach, academic detailing, and the use of local opinion leaders are the most consistently effective interventions reported. Interventions that are theory based, that incorporate two or more distinct strategies (i.e., that are multicomponent), or that do both are consistently more likely to work than single interventions. Moreover, the Internet, technologic platforms for social networking, and Web 2.0 applications can serve as important dissemination channels, allowing users to create and actively interact with information in ways that support intervention adoption, use, and implementation.
A recent narrative review of D & I research models identified 61 models. Models were sorted into three author-defined categories based on:
1. Construct flexibility: Rated on a scale of 1 to 5, where 1 was broad (loosely outlined and defined constructs) and 5 was operational (detailed, step-by-step actions for completion of the D & I research process) and with models falling in between scored as 2, 3, or 4.
2. Dissemination or implementation focus: defined as
a. Dissemination only (D-only): Focus on active approach of spreading evidence-based interventions to the target audience via determined channels using planned strategies
b. Dissemination = Implementation (D=I): equal focus on D & I
c. Implementation only (I-only): Focus on putting to use or integrating evidence-based interventions within a setting
3. Socioecologic framework: The level(s) of the socioecologic framework at which the model operates: individual, organization, community, or system.
The review identified 11 D-only models, 16 were combined dissemination and implementation models with a predominant focus on dissemination (D >I), 17 were D = I, five were combined dissemination and implementation models with a predominant focus on implementation (I >D), and 12 were I-only. The socioecologic level targeted by each model was variable and ranged from a systemwide orientation to community, organizational, individual, or policy levels. We present an example of a broad D = I model and an operational I-only model to illustrate construct choices available for researchers and practitioners in choosing a model to frame their work.
The Interactive Systems Framework (ISF) for Dissemination and Implementation is an integrated model developed by Wandersman and colleagues (2008) focused on the infrastructure and systems (e.g., practitioners, organizations that provide support to practitioners) needed for D & I to take place at multiple levels (e.g., system, community, organization, individual, and policy). The ISF is a broad model (score of 2) designed to accommodate multiple perspectives (e.g., the perspective of the funder, researcher) and includes the activities or functions carried out by people in multiple types of roles, highlighting the need for communication among different stakeholders in the system for D & I to be successful. Focused on prevention, ISF consists of three systems:
1. The Prevention Synthesis and Translation System (PSTS) is conceptualized as distilling information about innovations and preparing them for implementation by end users.
2. The Prevention Support System (PSS) is conceptualized as supporting the work of those who will put the innovations into practice.
3. The Prevention Delivery System (PDS) is focused on the implementation of innovations (e.g., delivery of programs) in the field.
Individuals and organizations using the ISF framework may conduct systematic reviews and meta-analyses as described in the PSTS to create evidence along with related tools and materials that translate evidence findings into key concepts and actionable messages that may be tailored for a particular audience. Examples include clinical practice guidelines issued by the AHRQ (http://www.ahrq.gov), CDC (http://www.cdc.gov), USPSTF (http://www.uspreventiveservicestaskforce.org), or Cochrane Collaboration (http://www.cochrane.org), professional organizations and societies representing a specific area of clinical practice. These organizations conduct a systematic review process, publish their findings, and design and disseminate tools and materials to inform patients, practitioners, and researchers about their findings. A recent example includes the 2014 publication of The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General along with its accompanying Executive Summary, Consumer Booklet, Fact Sheets, Video and Podcast Series and list of Partner Resources (http://www.surgeongeneral.gov/library/reports/50-years-of-progress/).
Other organizations may use alternative methods such as expert testimony and existing resources to define a major clinical or public health problem and present consensus recommendations detailing opportunities for improving practice and conducting research. The President’s Cancer Panel Annual Report 2012–2013: Accelerating HPV Vaccine Uptake: Urgency for Action to Prevent Cancer (http://deainfo.nci.nih.gov/advisory/pcp/annualReports/HPV/Acknowledgements.htm#sthash.7LHOnm9S.dpbs) was released in April 2014. The report is based on expert testimony and advice gathered in four U.S. cities in 2012 and 2013. The report makes the case for HPV vaccination using available evidence, describes the urgent need for action and details four goals for accelerating HPV vaccine uptake in the United States, and outlines high-priority research to advance prevention of HPV related cancers.
PSS activities could focus on either the creation or use of efficacious or effective strategies to build capacity and skills among individuals or organizations attempting to put research into practice. Evidence creators, program developers, or practice champions may provide either general capacity building such as learning about how evidence is created or found in a particular field or intervention-specific capacity building such as toolkits describing evidence-based approaches to increasing practitioner self-efficacy in offering HPV vaccines to young adults or their parents.
Activities in the PDS focus on overcoming implementation barriers or building on implementation strengths of individuals or organizations. These activities may be designed within the ISF or as part of an I-only framework such as the Consolidated Framework for Implementation Research (CFIR). The CFIR combines constructs across published theories with redundant or overlapping definitions into an overarching typology designed to promote both implementation theory development and a context for evaluation of implementation efforts.
The CFIR is an operational model (score = 4) composed of five major domains: intervention characteristics, inner and outer setting, characteristics of the individuals involved, and the process by which the implementation is accomplished. Eight characteristics of an intervention, including evidence strength and quality, are specified. The outer setting includes the economic, political, and social context within which an organization resides, and the inner setting includes features of structural, political, and cultural contexts through which the implementation process will proceed. Four constructs relate to outer setting (e.g., patient needs and resources), 12 constructs to the inner setting (e.g., culture, leadership engagement), and 5 relate to individual characteristics. Successful implementation involves an active change process aimed to achieve individual and organizational level use of the intervention as designed (e.g., fidelity) and eight constructs related to process (e.g., plan, evaluate, and reflect). For example, the President’s Cancer Panel recommends implementation strategies such as changing policy to allow pharmacists to administer the HPV vaccine and to remove financial barriers to vaccination. Within practices, changes are recommended to provide adequate reimbursement for HPV vaccines and administration, expand Healthcare Effectiveness Data and Information Set (HEDIS) measure regarding HPV vaccination to include adolescent males, and development of centralized immunization information systems that are interoperable and integrated with office-based EHRs.
SUMMARY
Evidence-based D & I approaches exist, should be used and evaluated when possible if practice or individual practitioner or patient change is desired. Research designed to compare the effectiveness of alternate D & I strategies is needed to both assess the relative advantage of one evidence-based strategy over another or the relative advantage of a new strategy compared with an existing evidence-based strategy. Care should be taken to determine and specify the desired endpoint or primary outcome, to choose and consistently use a known model and its constructs to frame the research question and evaluate relative effectiveness, and to engage the intended audience in the design and conduct of the research.
In summary, a greater focus on implementation and dissemination of scientific findings and evidence-based medical practices is essential to realizing potential gains from biomedical research and improving the quality and efficiency of health care. Recent developments to guide D & I science include the development and use of theories, frameworks, and models along with associated methods and metrics. Although great progress has been made, there is much work to be done. In particular, more consistency in terminology and better definition of outcome measures will be important to systematic progress in this area of incredible importance to public health and well-being.
1. Implementation science
A. seeks to understand the behavior of health care professionals and other stakeholders.
B. is the study of methods to promote the integration of research findings and evidence into health care policy and practice.
C. is an emerging field of growing importance to health care delivery.
D. is all of the above.
2. Issues most likely to interfere with implementation of effective health care interventions include
A. economic and behavioral issues.
B. spatiotemporal issues.
C. geopolitical issues.
D. mathematical probabilities.
3. Dissemination is:
A. a passive, informal approach to communication.
B. a formal, planned process with the intent of spreading knowledge.
C. a mechanism of reviewing an evidence base.
D. the preparatory phase before diffusion of information.
4. Implementation outcomes generally would NOT include
A. use of an intervention by an individual practitioner.
B. integration of an intervention within established practice.
C. citation index of an article.
D. use of an innovation within a community setting.
5. An intervention or innovation is more likely to be adopted if
A. it is easy to use.
B. it is based on credible evidence.
C. it has a clear, unambiguous advantage for the individual and system.
D. it can be tried on a limited basis before widespread adoption.
6. Organizational characteristics of large organizations that predict successful implementation of interventions or innovations include all but
A. absorptive capacity for new knowledge.
B. strong leadership and strategic vision.
C. decentralized decision-making structures.
D. well-designed data systems.
7. The Interactive Systems Framework describes three systems. Which system is not part of the ISF?
A. Prevention Synthesis and Translation System
B. Prevention Awareness and Communication System
C. Prevention Support System
D. Prevention Delivery System
8. HPV vaccination rates lag behind those in other countries for which reasons?
A. Parental and provider knowledge and attitudes about the vaccine
B. Parental concerns about vaccine safety
C. Providers’ lack of familiarity with burden of disease associated with HPV-related cancers
D. Documented side effects of the vaccine
9. Recent developments to guide dissemination and implementation science include all but which of the following?
A. The development of theories, frameworks, and models
B. Creation of model-driven methods and metrics
C. Compilations of data from D & I studies
D. Head-to-head comparisons of methods and metrics
10. Which of the following is not an intended outcome of dissemination?
A. Promote the integration of research findings and evidence into health care policy and practice
B. Increase motivation to use and apply evidence
C. Increase reach to a variety of audiences
D. Increase ability to actually use and apply evidence
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree