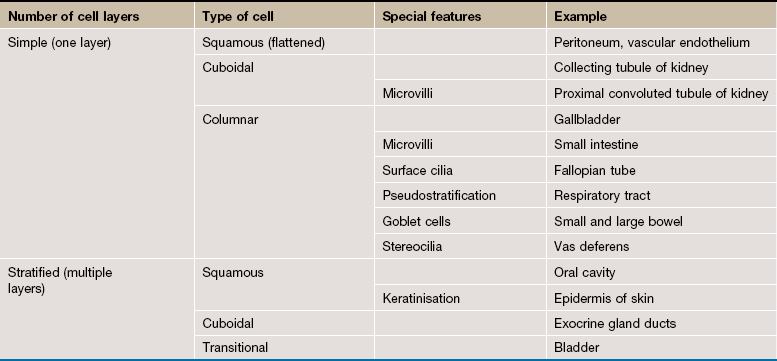
5 The epithelia (singular: epithelium) are a diverse group of tissues that include both surface epithelia and solid organs. Surface epithelia cover or line all body surfaces, cavities and tubes and form the interface between different biological compartments. For instance, the epidermis of the skin is exposed to the external environment and the epithelial lining of the gastrointestinal tract is exposed to partially digested food and bacteria in the lumen of the gut. Functions of epithelia include: forming a protective barrier, regulation of the exchange of molecules between compartments (selective diffusion and absorption) and synthesis and secretion of glandular products. Many of these major functions may be exhibited at a single epithelial surface. For example, the epithelial lining of the small intestine is primarily involved in absorption of the products of digestion, but the epithelium also protects itself from noxious intestinal contents by secreting a surface coating of mucus. Epithelial cells are characterised by the production of keratin intermediate filaments (see Ch. 1), and this can be used to recognise epithelial cells using immunohistochemistry, a technique often used in diagnostic histopathology to classify difficult malignant tumours (see Appendix 2). Surface epithelia form continuous sheets comprising one or more layers of cells. Epithelial cells are bound to adjacent cells by a variety of cell junctions that provide physical strength and mediate exchange of information and metabolites. All epithelia are supported by a basement membrane (see Ch. 4) which separates the epithelium from underlying supporting tissues. Thus epithelial cells are polarised, with one side facing the basement membrane and underlying supporting tissues (the basal surface) and the other facing outwards (the apical surface). FIG. 5.1 Simple squamous epithelium FIG. 5.2 Simple cuboidal epithelium FIG. 5.3 Simple columnar epithelium FIG. 5.4 Simple columnar ciliated epithelium FIG. 5.5 Pseudostratified columnar ciliated epithelium FIG. 5.6 Stratified squamous epithelium FIG. 5.7 Stratified cuboidal epithelium FIG. 5.8 Transitional epithelium
Epithelial tissues
Introduction
Simple Epithelia
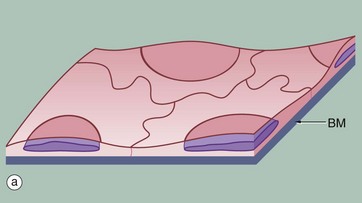
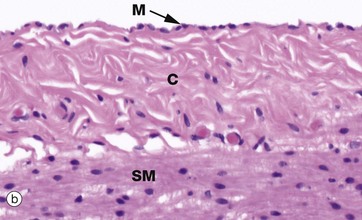
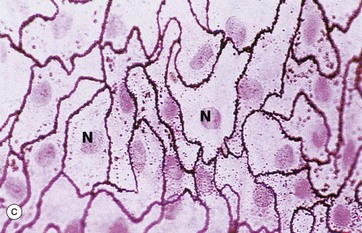
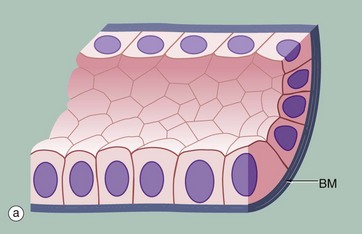
(a) Diagram (b) H&E (HP) (c) Spread preparation, silver method/neutral red (HP)
Simple squamous epithelium is composed of flattened, irregularly shaped cells forming a continuous surface that is sometimes called pavemented epithelium; the term squamous derives from the comparison of the cells to the scales of a fish. Like all epithelia, this delicate lining is supported by an underlying basement membrane BM as shown diagrammatically.
Simple squamous epithelium is found lining surfaces involved in passive transport (diffusion) of either gases (as in the lungs) or fluids (as in the walls of blood capillaries). Simple squamous epithelium also forms the delicate lining of the pleural, pericardial and peritoneal cavities where it allows passage of tissue fluid into and out of these cavities. Although these cells appear simple in form they have a wide variety of important roles.
Micrograph (b) shows a mesothelium (peritoneum) covering the surface of the appendix and illustrates the typical appearance of simple squamous epithelium in section. The mesothelial lining cells M are so flattened that they can only be recognised by their nuclei, which bulge on the surface. The supporting basement membrane is thin and, in H&E stained preparations, has similar staining properties to the underlying collagenous supporting tissue C; hence it cannot be seen in this micrograph. Deeper in the wall of the appendix, the smooth muscle SM of the muscularis propria can be identified.
In the preparation used in micrograph (c), the mesothelial lining of the peritoneal cavity has been stripped from the underlying tissues and spread onto a slide, thus permitting a surface view of simple squamous epithelium. The intercellular substance has been stained with silver thereby outlining the closely interdigitating and highly irregular cell boundaries. The nuclei N are stained a slightly darker pink.
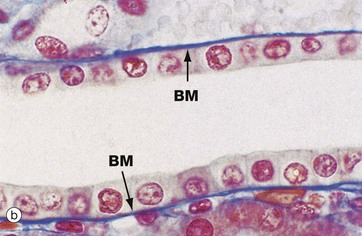
(a) Diagram (b) Azan (HP)
Simple cuboidal epithelium represents an intermediate form between simple squamous and simple columnar epithelium; the distinction between tall cuboidal and low columnar is often arbitrary and is of descriptive value only. In the section perpendicular to the basement membrane BM, the epithelial cells appear square, leading to its traditional description as cuboidal epithelium; on surface view, however, the cells are actually polygonal in shape. The nucleus is usually round and located in the centre of the cell.
Simple cuboidal epithelium usually lines small ducts and tubules that may have excretory, secretory or absorptive functions; examples are the collecting tubules of the kidney and the small excretory ducts of the salivary glands and pancreas.
Micrograph (b) shows the cells lining a collecting tubule in the kidney. Although the boundaries between individual cells are indistinct, the nuclear shape provides an approximate indication of the cell size and shape. The underlying basement membrane BM appears as a prominent blue line with the Azan staining method, in contrast to basement membranes stained with the standard H&E stain (see Fig. 5.3b) that are generally indistinguishable.
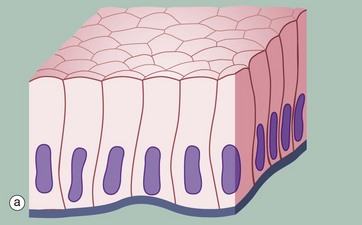
(a) Diagram (b) H&E (HP)
Simple columnar epithelium is similar to simple cuboidal epithelium except that the cells are taller and appear columnar in sections perpendicular to the basement membrane. The height of the cells may vary from low to tall columnar, depending on the site and/or degree of functional activity. The nuclei are elongated and may be located towards the base, the centre or occasionally the apex of the cytoplasm; this is known as the polarity of the nucleus. Simple columnar epithelium is found on absorptive surfaces such as in the small intestine, as well as at secretory surfaces such as that of the stomach.
Micrograph (b) shows simple columnar epithelium taken from the endocervix where it has the function of secreting mucus. Note the typically basally located nuclei.
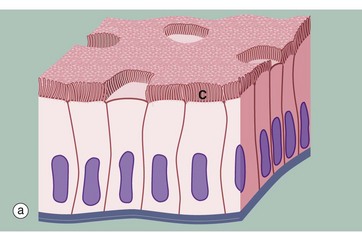
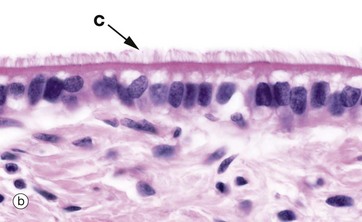
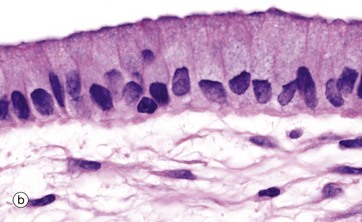
(a) Diagram (b) H&E (HP)
Some simple columnar epithelia have surface cilia C on the majority of the cells (see also Fig. 5.13). Among the ciliated cells are scattered non-ciliated cells that usually have a secretory function.
Cilia are much larger than microvilli (see Fig. 5.14) and are readily visible with the light microscope. Each cilium consists of a finger-like projection of the plasma membrane, its cytoplasm containing modified microtubules. Each cell may have up to 300 cilia that beat in a wave-like manner, synchronised with the adjacent cells. The waving motion of the cilia propels fluid or minute particles over the epithelial surface. Simple columnar ciliated epithelium is found mainly in the female reproductive tract. Micrograph (b), taken from the Fallopian tube (oviduct), shows one of its numerous folds covered by simple columnar ciliated epithelium. The predominant cell type in this epithelium is tall columnar and ciliated, the nuclei being located towards the midzone of the cells. The less numerous blue-stained cells with basally located nuclei are not ciliated and have a secretory function. Ciliary action facilitates transport of the ovum from the ovary towards the uterus.
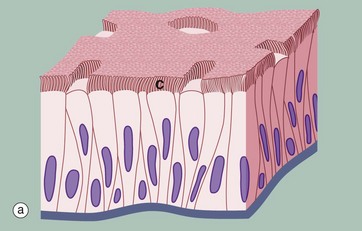
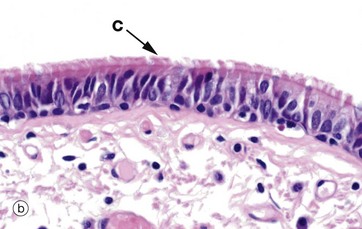
(a) Diagram (b) H&E (MP)
Another variant of simple columnar epithelium is described in which the majority of cells are also usually ciliated C. The term pseudostratified is derived from the appearance of this epithelium in section, which conveys the erroneous impression that there is more than one layer of cells. In fact, this is a true simple epithelium, since all the cells rest on the basement membrane. The nuclei of these cells, however, are disposed at different levels, thus creating the illusion of cellular stratification. Scattered stem cells (see Ch. 2) are found throughout the epithelium; these generally are devoid of cilia (i.e. less differentiated) and do not extend to the luminal surface.
Pseudostratified columnar ciliated epithelium may be distinguished from true stratified epithelia by two characteristics. Firstly, the individual cells of the pseudostratified epithelium exhibit polarity, with nuclei being mainly confined to the basal two-thirds of the epithelium. Secondly, cilia are never present on true stratified epithelia.
Pseudostratified epithelium is almost exclusively confined to the airways of the respiratory system in mammals and is therefore often referred to as respiratory epithelium. Micrograph (b) illustrates the lining of a bronchus. In the respiratory tract, the cilia propel a surface layer of mucus containing entrapped particles towards the pharynx in what is often described as the mucociliary escalator. The mucus is secreted by nonciliated goblet cells found amongst the ciliated cells (not seen in this micrograph, see Figs 5.16 and 5.17).
Stratified Epithelia
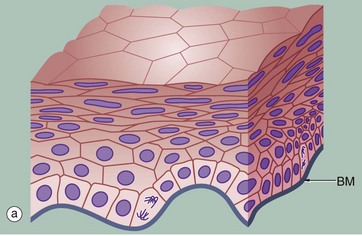
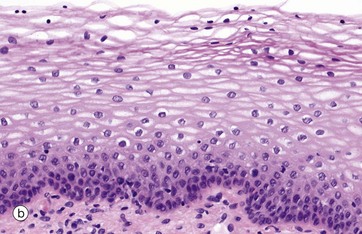
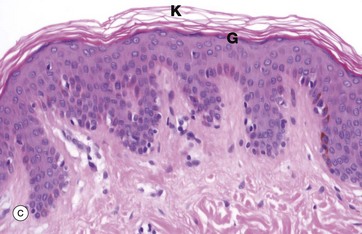
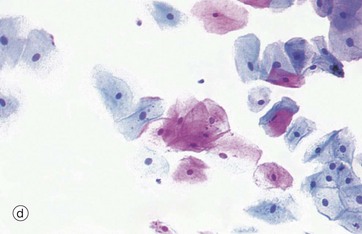
(a) Diagram (b) H&E (HP) (c) H&E (MP) (d) Papanicolaou (HP)
Stratified squamous epithelium consists of a variable number of cell layers that exhibit maturation from a cuboidal basal layer to a flattened surface layer. The basal cells which are adherent to the underlying basement membrane include continuously dividing stem cells, their offspring migrating towards the surface where they are ultimately shed as anucleate squames. Stratified squamous epithelium is adapted to withstand abrasion, with plentiful cell junctions and a prominent intermediate filament (keratin) cytoskeleton. This type of epithelium lines the oral cavity, pharynx, oesophagus, anal canal, uterine cervix and vagina, sites which are subject to mechanical abrasion but which are kept moist by glandular secretions, such as the salivary glands of the mouth.
The epithelium in micrograph (b) is from the uterine cervix. Note the cuboidal basal layer and the maturation through the large polygonal cells of the intermediate layers to the flattened superficial squamous cells. The cytoplasm in these cells often appears clear due to the glycogen content.
Keratinising stratified squamous epithelium (c) constitutes the epithelial surface of the skin (the epidermis) and is adapted to withstand the constant abrasion and desiccation to which the body surface is exposed. During maturation, the epithelial cells accumulate keratin intermediate filaments which are cross-linked with proteins such as involucrin and loricrin in a process called keratinisation (or cornification). This results in the formation of a tough, non-living surface layer (stratum corneum) consisting of a compacted cross-linked keratin matrix K interspersed with specialised lipids (see Ch. 9). The underlying granular cell layer G consists of epithelial cells with extensive tight junctions, forming a waterproof barrier. The nuclei of the maturing epithelial cells become progressively condensed (pyknotic) and eventually disappear along with the other cellular organelles. Keratinisation may be induced in normally non-keratinising stratified squamous epithelium such as that of the oral cavity when exposed to excessive abrasion (e.g. poorly-fitting false teeth).
Micrograph (d) shows a smear made from normal cells scraped from the uterine cervix as it projects into the vagina. The degenerate, scaly superficial cells stain pink with this staining method, while the living cells from deeper layers stain blue. This is the basis of the well-known ‘Pap smear’ which examines cytological preparations of cervical cells for pre-cancerous changes.
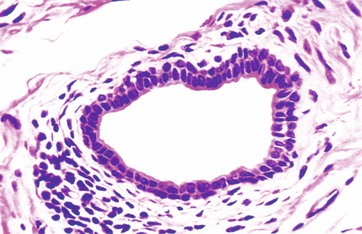
H&E (HP)
Stratified cuboidal epithelium is a thin, stratified epithelium that usually consists of only two or three layers of cuboidal cells. This type of epithelium is usually confined to the lining of the larger excretory ducts of exocrine glands such as the salivary glands. Stratified cuboidal epithelium is probably not involved in significant absorptive or secretory activity but merely provides a more robust lining than would be afforded by a simple epithelium.
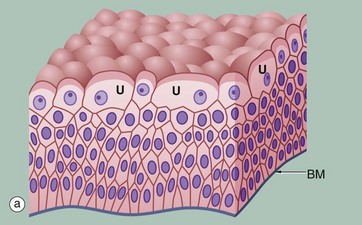
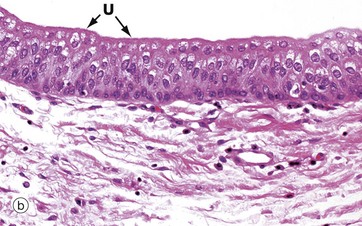
(a) Diagram (b) H&E (HP)
Transitional epithelium (or urothelium) is a form of stratified epithelium found only in the urinary tract in mammals, where it is highly specialised to accommodate a great degree of stretch and to withstand the toxicity of urine. This epithelial type is so named because it has some features intermediate (transitional) between stratified cuboidal and stratified squamous epithelia. In the non-distended state, transitional epithelium appears to be about four to five cell layers thick. The basal cells are roughly cuboidal, the intermediate cells are polygonal and the surface cells (umbrella or dome cells U) are large and rounded and may contain two nuclei. In the stretched state, transitional epithelium often appears only two or three cells thick (although the actual number of layers remains constant) and the intermediate and surface layers are extremely flattened.
Micrograph (b) shows the appearance of transitional epithelium from the lining of a non-distended bladder. The shape and apparent size of the basal and intermediate cells vary considerably depending on the degree of distension, but the cells of the surface layer usually retain characteristic features. Firstly, the surface umbrella cells are large and pale stained with a scalloped surface outline often overlapping two or more of the underlying cells. Secondly, the luminal surface of the cells appears thickened and more densely stained.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine