The purpose of the cardiovascular system is to ensure perfusion of the tissues with blood, allowing for the delivery of nutrients and oxygen, and the removal of metabolites including CO2. This is achieved by the systemic circulation, which delivers oxygenated blood via arteries and then arterioles (<50 µm in diameter) to the capillary network, where exchange occurs.
Regulation of vascular tone
Blood flow is driven by the increased pressure generated by the heart. Blood readily flows through low-resistance conduit arteries (e.g. the aorta then the superior mesenteric artery) to the tissues and organs. At this point the control of blood flow, and therefore tissue, perfusion is determined by vascular resistance. This impedes flow, meaning that blood follows the route of least resistance and is facilitated by vasodilatation and opposed by vasoconstriction.
Vascular resistance is determined by Poiseuille’s law:
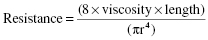
Therefore vascular resistance is proportional to 1/radius4, meaning that small decreases in radius lead to substantial increases in vascular resistance. Hence, small changes in vessel diameter, governed by vascular tone, have profound effects on blood flow and pressure.
Autonomic control of vascular tone
One of the key regulators of arterial diameter and resistance is the sympathetic nervous system. Sympathetic nerve fibres release noradrenaline, which activates α1-adrenoceptors on the vascular smooth muscle, leading to an increase in intracellular Ca2+ via release from stores and Ca2+ influx via L-type calcium channels. This leads to vasoconstriction and increases vascular resistance. Sympathetic innervation and circulating adrenaline also stimulate β2-adrenoceptors (coupled via adenylyl cyclase to cAMP), largely associated with arteries supplying skeletal muscle, leading to vasodilatation, which results in increased blood flow, for example during exercise (Figures 31.1 and 31.2).
Sympathetic control is also augmented by angiotensin II (AII) (Chapter 32) from the renin-angiotensin system. This system is activated by both indications of low blood pressure and sympathetic stimulation, and results in the release of renin by the juxtaglomerular (granular) cells of the kidney.
Endothelial autacoids and vascular control
The vascular endothelium is now recognised as a key regulator of vascular tone by the release of endothelium-derived autacoids (Figure 31.1). The archetypical endothelium-derived relaxant is the gas nitric oxide (NO), which is derived from L-arginine via NO synthase. There is a tonic release of NO, which helps to modulate vascular resistance and control blood pressure. The release of NO also occurs in response to agonists and shear stress resulting from blood flow. This leads to flow-dependent dilatation to match blood flow to demand. NO acts on the vascular smooth muscle to stimulate guanylyl cyclase, which increases levels of cGMP, resulting in vasodilatation.
The endothelium also releases the prostanoid, prostacyclin (PGI2), and the so-called endothelium-derived hyperpolarising factor (EDHF), which also causes vasodilatation. The activity of EDHF may, in part, be explained by the transfer of electrical current (hyperpolarisation) via gap junctions to the vascular smooth muscle.
The endothelium also releases peptides of the endothelin family, which are the most potent vasoconstrictors known.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


