7 CASE 7
PATHOPHYSIOLOGY OF KEY SYMPTOMS
Arterial blood pressure is sensed by the stretch receptors of the aortic arch and the carotid sinus, collectively called arterial baroreceptors. A drop in arterial blood pressure unloads the baroreceptors and causes a sympathetic activation and a parasympathetic inhibition (Fig. 7-1). Sympathetic activation causes increases in heart rate, ventricular contractility, and total peripheral resistance and a decrease in venous capacitance (Table 7-1). These changes cause an increase in cardiac output and a reduction in the volume of blood exiting the arteries. Consequently, arterial pressure recovers toward normal.
TABLE 7–1 Autonomic Effects on Various Organs of the Body
| Organ | Effect of Sympathetic Stimulation | Effect of Parasympathetic Stimulation |
|---|---|---|
| Eye | ||
| Pupil | Dilated | Constricted |
| Ciliary muscle | Slight relaxation (far vision) | Constricted (near vision) |
| Glands | Vasoconstriction and slight secretion | Stimulation of copious secretion (containing many enzymes for enzyme-secreting glands) |
| Nasal | ||
| Lacrimal | ||
| Parotid | ||
| Submandibular | ||
| Gastric | ||
| Pancreatic | ||
| Sweat glands | Copious sweating (cholinergic) | Sweating on palms of hands |
| Apocrine glands | Thick, odoriferous secretion | None |
| Blood vessels | Most often constricted | Most often little or no effect |
| Heart | ||
| Muscle | Increased rate | Slowed rate |
| Increased force of contraction | Decreased force of contraction (especially of atria) | |
| Coronaries | Dilated (β2); constricted (α) | Dilated |
| Lungs | ||
| Bronchi | Dilated | Constricted |
| Blood vessels | Mildly constricted | ? Dilated |
| Gut | ||
| Lumen | Decreased peristalsis and tone | Increased peristalsis and tone |
| Sphincter | Increased tone (most times) | Relaxed (most times) |
| Liver | Glucose released | Slight glycogen synthesis |
| Gallbladder and bile ducts | Relaxed | Contracted |
| Kidney | Decreased output and renin secretion | None |
| Bladder | ||
| Detrusor | Relaxed (slight) | Contracted |
| Trigone | Contracted | Relaxed |
| Penis | Ejaculation | Erection |
| Systemic arterioles | ||
| Abdominal viscera | Constricted | None |
| Muscle | Constricted (adrenergic α) | None |
| Dilated (adrenergic β2) | ||
| Dilated (cholinergic) | ||
| Skin | Constricted | None |
| Blood | ||
| Coagulation | Increased | None |
| Glucose | Increased | None |
| Lipids | Increased | None |
| Basal metabolism | Increased up to 100% | None |
| Adrenal medullary secretion | Increased | None |
| Mental activity | Increased | None |
| Piloerector muscles | Contracted | None |
| Skeletal muscle | Increased glycogenolysis | None |
| Increased strength | ||
| Fat cells | Lipolysis | None |
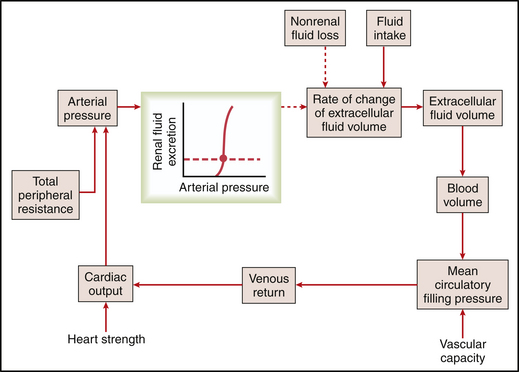
The initial event in this patient was the loss of circulating blood volume. Estimated blood volume for this individual is 5 L, which accounts for 8% of body weight. Blood loss caused a drop in venous volume and venous pressure and, consequently, a fall in cardiac preload (see Fig. II-2, p. 21). The fall in preload causes a drop in cardiac output and, therefore, a drop in arterial blood pressure (Fig. 7-2).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


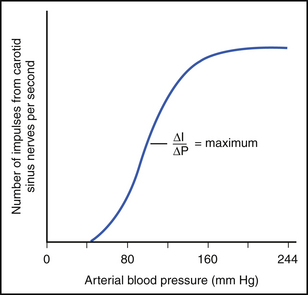
 I, change in carotid sinus nerve impulses per second;
I, change in carotid sinus nerve impulses per second;  P, change in arterial blood pressure in millimeters of mercury.
P, change in arterial blood pressure in millimeters of mercury.